The cardiovascular system
· The cardiovascular represents “Cardio” means Heart; to ensure constant circulation of blood and “Vascular” means Blood Vessel; through which the blood flows.
· The heart is pumped by two circulation systems;
1. The pulmonary circulation
2. The systemic circulation

Fig. 02: Blood circulation
The heart and Homeostasis
· The heart contributes homeostasis by pumping blood through blood vessels to the body to deliver oxygen and nutrients and removes wastes.
Some key facts
· The heart beats 1,00,000 times every day.
· 35 million beats/year, 2.5 billion/average lifetime.
· The heart pumps blood through on estimated 1,20,000 km. of blood vessels.
· During sleeping the heart pumps about 5 liters of blood to the lungs and same to the rest of the body. In a day pumps about 14,000 liters and in a year 5 million liters of blood pumped.
· The scientific study of heart is called cardiology
· Homeostasis: A state of steady internal, physical and chemical condition maintained by living system.
Anatomy of heart
· The heart is a rough cone shaped hollow muscular organ, about 10 cm long and is about the size of the owner’s fist.
· The weight of the adult male heart is 310gm and female heart is 225gm.
· The heart is lies in the thoracic cavity in the mediastinum.
Organ associated with the heart
· Inferiorly : Apex
· Superiorly : Aorta, Superior Vena Cava, Pulmonary artery, and Pulmonary veins
· Posteriorly : Esophagus, Descending aorta, Inferior Vena Cava, Trachea, Left and
Right Bronchus, and Thoracic vertebrae
· Laterally : The lungs
· Anteriorly : Sternum, Ribs, and Intercostal Muscle.
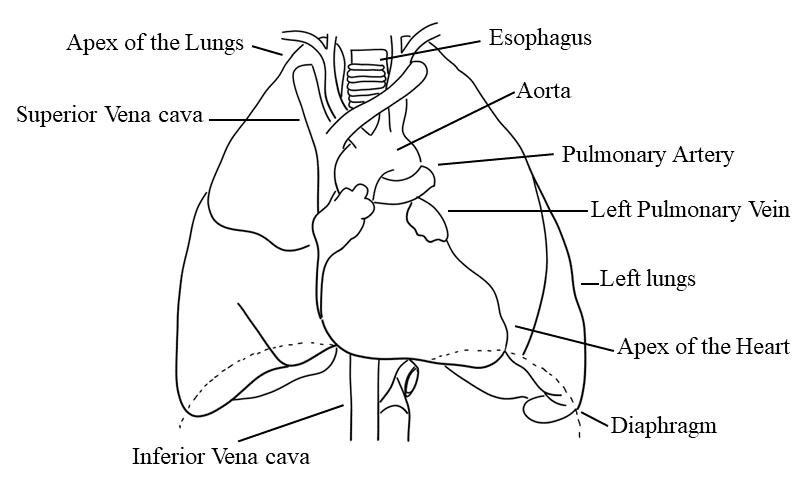
Fig. 02: Organ associated with the heart
STRUCTURE OF HEART (THE HEART WALL)
Endocardium | Myocardium | Epicardium |
· The inner most layer of the heart. · It lines cavities and valve of the heart. · Structurally: loose connective tissue and simple squamous connective tissue. Connective tissue 1. Subendothelial connective tissue · Loose connective tissue rich in elastic fibre and collagen fibre. 2. Dense connective tissue · Rich in collagen fibre | · Middle layer of the heart · The myocardium is composed if cardiac muscle and is an involuntary striated muscle. · This layer is responsible for contraction of the heart. | · The outermost layer and is made up two sac. · The outer sac consists of fibrous tissue and the inner of a continuous double layer of serous membrane.
|
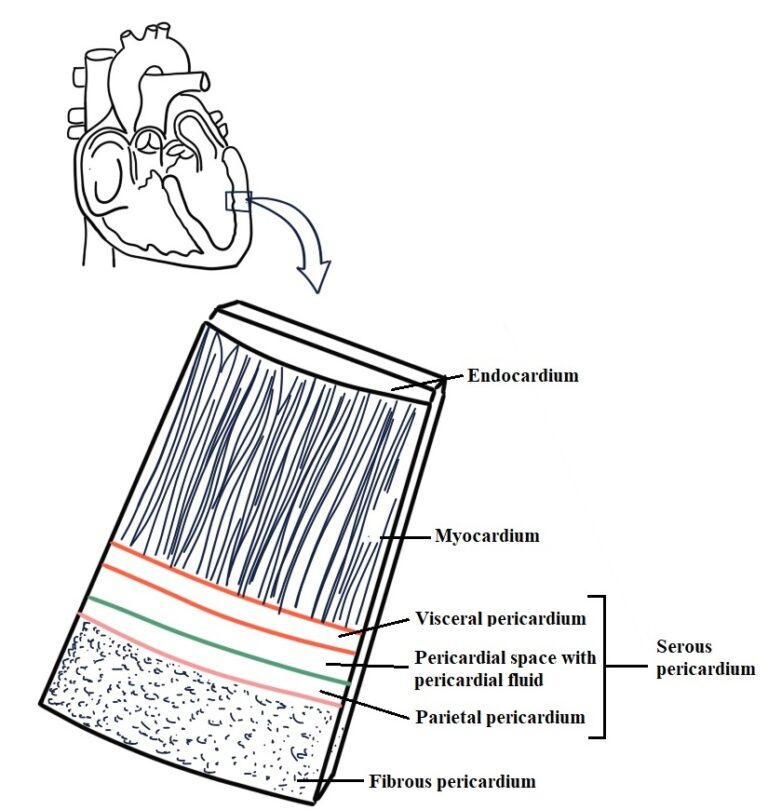
Fig. 03: The heart wall
Structure of heart
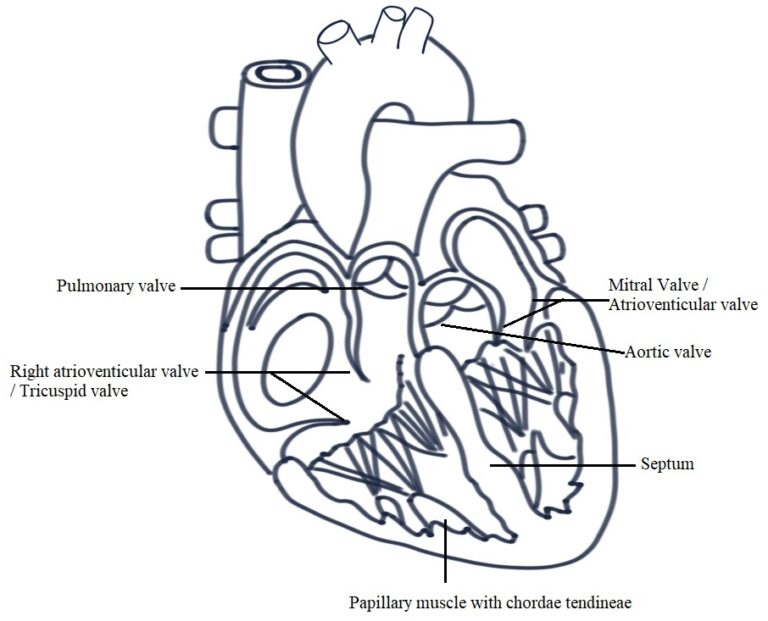
Fig. 04: Internal structure of the Heart
CHAMBERS
· The walls of the heart consist of cardiac muscle called myocardium.
· The heart consist of 4 chambers are lined with endocardium.
· The upper chambers of the heart are right and left atria (Atrium).
· The atria are relatively thin wall and are separated by a wall called interatrial septum.
· The lower chambers of the heart are right and left ventricles, which have thicker walls and are separated by the interventricular septum.
Right atrium
· The blood from the body is returned to the right atrium by the two major caval veins.
· Blood from upper limbs is carried by superior vena cava whereas, blood from the lower body is carried by inferior vena cava.
· From the right atrium, blood will flow through the atrioventricular valve (AV Valve) / Tricuspid valve into the right ventricle.
· The tricuspid valve is made of three flaps (cups) of endocardium and connective tissue.
· The main purpose of the valves is to prevent backflow of the blood.
Left atrium
· The left atrium receive blood from the lungs by pulmonary veins.
· This blood will then flow into the left ventricle through left atrioventricular valve / Mitral valve / Bicuspid valve.
· It prevents backflow of blood from the left ventricle to the left atrium.
Right ventricle
· Contraction of right ventricle, the tricuspid valve closes and the blood is pumped to the lungs through pulmonary artery.
· The flow of blood from right ventricle to pulmonary artery is regulated by pulmonary semilunar valve.
Left ventricle
· Thicker than the right ventricle.
· The left ventricle pumps blood to the body through aorta, the largest artery of the body.
· Aortic semilunar valve opened by the force of contraction of left ventricle, which also closes the mitral valve and prevent the back flow of blood.
BLOOD FLOW THROUGH THE HEART
· The deoxygenated blood from upper limbs drains into right atrium through superior vena cava and lower limbs blood through inferior vena cava into the right atrium.
· This blood passes into the right ventricle via right atrioventricular valve (tricuspid valve) and from there is pumped into pulmonary artery or trunk.
· The opening of pulmonary artery is guarded by the pulmonary valve, formed by semilunar valve/cups. This valve prevents the backflow of blood into the right ventricle when ventricular muscle relaxes.
· The pulmonary artery divided into left and right pulmonary artery, which caries venous blood to the lungs where exchange of gases takes place (CO2 and O2).
· Two pulmonary veins from each lung carry oxygenated blood back to the left atrium.
· The blood then passes through the left atrioventricular valve into the left ventricle and from there it is pumped into the aorta (the first arty of the general circulation).
· The opening of the aorta is guarded by the aortic valve formed by three semilunar cups.
Arterial supply
· The right and left coronary artery which split from aorta just distal to the aortic valve, supply the heart with arterial blood.
· Coronary artery receives about 5% of blood pumped from the heart.
· Coronary artery then forming a vast network of capillaries.
Venous drainage
· A number of cardiac veins that joins to form the coronary sinus, which open into the right atrium. The remainder passes directly into the heart chambers through little venous channels.
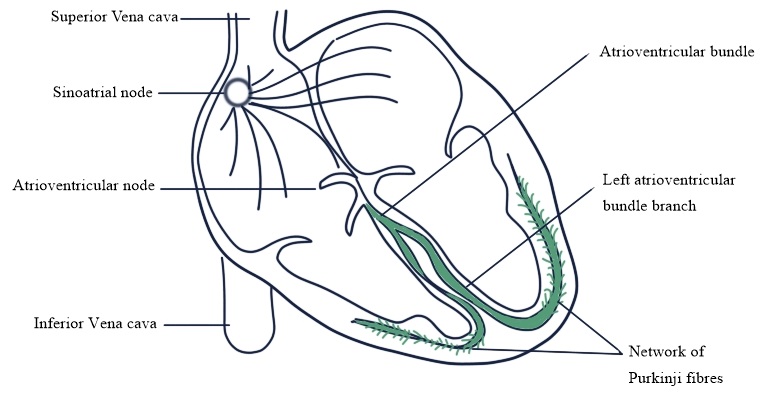
CONDUCTING SYSTEM
SA node
· Sinoatrial node is a small mass of specialised cells lies in the wall of the right atria near opening of superior vena cava.
· It regulates electrical impulses, maintain depolarization (60-80 beats/min) is followed by repolarization.
· Also called pacemaker of the heart.
· Firing of the SA node triggers atrial contraction.
AV node
· Atrioventricular node is a small mass of neuromuscular tissue is situated in the wall of the atrial septum near the atrioventricular valves.
· Transmit electrical current into the ventricles.
· The action starts when the atrial finish contracting before the ventricle starts.
· Act as secondary pacemaker function when SA node not working properly (40-60 beats/min).
Bundle of His
· It is a mass of specialised fibre that originated from the atrioventricular node.
· The AV bundle crosses the fibrous ring that separates atria and ventricle.
· It is divides into right and left bundle branches.
· Within the ventricular myocardium the branches break up into fine fibres called purkinje fibres.
· AV bundle, Bundle branches and purkinje fibres transmit electrical impulses from A-V node to the apex of the myocardium (Ventricular contraction).
NERVE SUPPLY TO THE HEART
· It influenced by autonomic nerve (sympathetic and parasympathetic) originated in the cardiovascular centre in the medulla oblongata.
· Vagus nerve (parasympathetic) supply mainly the SA and AV nodes and atrial muscle (Decrease heart rate↓).
· Sympathetic nerve supplies the SA and AV nodes and the myocardium of atria and ventricles (Increase heart rate↑).
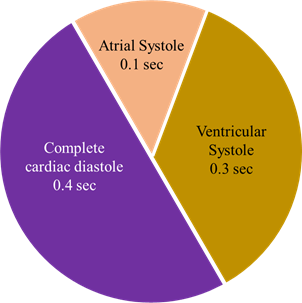
THE CARDIAC CYCLE
· A rest healthy heart is beat at a rate of 60-80bpm.
· During cardiac cycle the heart contract and then relaxes.
· Contraction – Systole
· Relaxation – Diastole
· When heart rate is 75 b/min, a cardiac cycle lasts 0.8 sec.
Atrial systole
· It lasts about 0.1 sec.
o Atria – contraction
o Ventricle – relaxation
· Depolarization of SA node
↓
Atria contraction
↓
Opening of AV valve into the ventricles
· Atrial systole pushes 25 ml of blood into the ventricle and ventricle contains 105 ml of blood. The total blood is 130 ml this condition is called end diastolic volume (end of the ventricular relaxation → diastole)
Ventricular systole
· Lasts about 0.3 sec.
· Ventricles are contracting at the same time atria are relaxed (atrial diastole).
· Ventricular depolarization
↓
Closing of semilunar and AV valves (Isovolumetric contraction)
↓
Same ventricular volume
↓
Continued contraction of the ventricles
↓
Left ventricle → pressure increases to 80mmHg (Aortic pressure)
↓
Right ventricle → pressure rises to 20 mmHg
↓
Both semilunar valve open
↓
Ventricular ejection (about 0.25 sec last)
↓
Pressure continue (left ventricle) to about 120 mmHg
↓
25-30 mmHg → right ventricle
· Left ventricle ejects about 70 ml blood into the aorta and same volume of blood into the pulmonary trunk.
Complete cardiac diastole
· Lasts about 0.4 sec.
· Atrial and ventricles are both relaxed.
· As ventricles relax → pressure within the chamber falls and blood flow back from aorta and pulmonary trunk.
· The semilunar valve closes and produce dicrotic wave
The heart sounds
· During each cardiac cycle the first sound is “Lub” is fairly loud and due to the closure of the AV Valves (Ventricular systole).
· The second sound “Dup” is softer and is due to the closure of the aortic and pulmonary valves (Ventricular diastole).
Electrical changes in the heart
· The electrical activity within the heart can be detected by attaching electrodes to the limbs and chest.
· The pattern of electrical activity may be displayed on an oscilloscope screen or traced on paper.
· The apparatus used is an electrocardiogram (ECG).
· Normal ECG showing five waves P, Q, R, S, T.
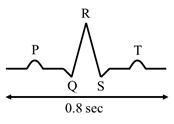
·
P
wave : Atrial depolarization; electrical
impulse from SA node.
·
QRS
complex: Ventricular depolarization; Impulse spread from AV node to AV bundle
to purkinje fibre.
·
T
wave: Ventricular repolarization.
Cardiac output
·
Cardiac
output is the amount of blood eject from each ventricle every minute.
·
The
amount of blood expelled by each contraction of each ventricles is stroke
volume.
·
CO
= Stroke volume × Heart rate
Stroke volume
·
It
determines by the volume of blood in the ventricle (VEDV) also called preload.
It depends on the amount of blood returning to the heart through venous return.
·
Increase
preload → more myocardial contraction
↓
Increase stroke volume, ↑CO
·
↑sympathetic
activity
·
↑Adrenalin,
Nor-adrenalin, thyroxine
Regulation of blood
pressure
|
Short term |
Intermediate term |
Long term |
|
→ Baroreceptor → Chemoreceptor → CNS ischemic response |
→ Capillary fluid shift → Stress relaxation |
→ Renal body fluid mechanism → Renin angiotensin system |
·
Blood
pressure is the force or pressure that the blood exerts on the walls of the
blood vessels.
·
If
it is too high → blood vessel can be damaged
→ Causing blood clots
·
If
it become too low → blood flow through tissue beds may be inadequate.
Systemic arterial blood
pressure
·
It
is the discharge of blood from the left ventricle into the aorta.
·
Blood
pressure usually higher in women than in men.
Systolic and diastolic
pressure
·
When
left ventricle pumps blood into aorta, the pressure produce within the arterial
system is called systolic blood pressure (120 mmHg).
·
When
complete cardiac diastolic occurs and the heart s become rest, the pressure
within the arteries is much lower and is called diastolic blood pressure (80
mmHg).
·
The
difference between systolic and diastolic blood pressure is the pulse pressure.
·
BP
= 120/80 mmHg or 16/11 kpa
Factor determine blood
pressure
·
Blood
pressure is determined by Co and peripheral resistance.
·
BP
= CO × Peripheral resistance
Peripheral or arteriolar
resistance
·
Arterioles
are the smallest arteries and they have a tunica media composed almost entirely
of smooth muscle, which responds to nerve and chemical stimulation.
·
Vasodilation
→ decrease in blood pressure
·
Vasoconstriction
→ increase in blood pressure
·
In
the older age tunica media is replaced by inelastic fibrous tissue → increase
blood pressure.
Autoregulation
·
The
organs of the body are capable of adjusting blood flow and blood pressure in
their own local vessels inadequately of systemic blood pressure. Also depends
on level of activities and body position, these properties are called autoregulation.
Sort term blood pressure regulation
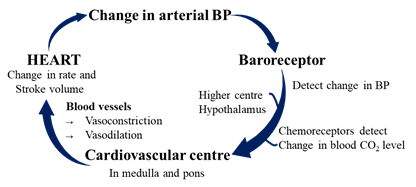
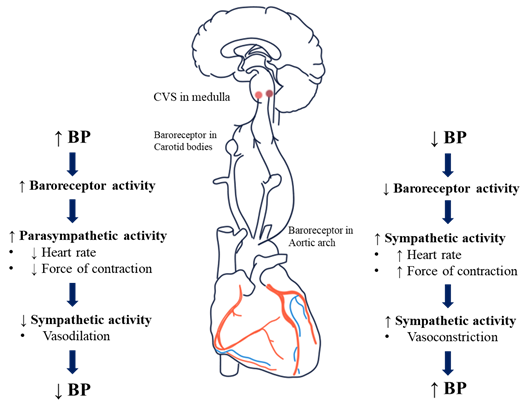
· Cardiovascular centre sends autonomic nerve (sympathetic and parasympathetic) to the heart and blood vessels.
· Baroreceptors are situated in arch of aorta and carotid sinus.
· Baroreceptors are a type of mechanoreceptor that detect the pressure of blood. They send message to the CNS to increase or decrease total peripheral resistance and cardiac output.
· Baroreceptors act intermediately as part of a negative feedback mechanism called baroreflex.
Chemoreceptor
· These are the nerve ending situated in the carotid and aortic bodies.
· It primarily worked in the control in the control of respiration.
· Chemoreceptors are sensitive to change in the level of CO2, O2 and acidity of blood pH.
· When it detected by chemoreceptors, they send signal to the CVS, which then increases sympathetic drive.
· Increase blood supply → increase O2 level.
· It influences its output when severe disruption of respiratory function or when arterial BP falls to less than 80 mmHg.
· Also found on the brain surface of the medulla oblongata, they measure CO2, O2 levels and pH of the cerebrospinal fluid.
Higher centres in the brain
· It influenced by emotional states such as fear, anxiety, pain and anger that stimulate changes in blood pressure.
INTERMEDIATE MECHANISM
Capillary fluid shift phenomenon
· Whenever there is an increase in blood pressure more fluid is filtered through the capillary wall into the interstitial space.
· Blood volume decreases and so blood pressure decreases.
· Reverse changes take place when blood pressure falls.
LONG TERM BLOOD PRESSURE REGULATION
· Long-term blood pressure regulation is mainly exerted by renin-angiotensin-aldosterone system (RAAS) and the action of antidiuretic hormone (ADH).
· Both of the system regulates blood volume, thus influencing blood pressure

PULSE
· The pulse is a wave of distension and elongation fact in an artery wall each time the left ventricle eject blood into the system.
· Each contraction of the left ventricle forces about 60-80ml of blood into the arterial system.
· The pulse can be felt at the wrist, side of the neck, back of the knees, top of the foot, groin, and where an artery is close to the skin.
BLOOD VESSELS
· Blood vessels varies in structure, size and function, there are;
→ Arteries
→ Arterioles
→ Capillaries
→ Venules
→ Veins
ARTERIES AND ARTERIOLES
· These are the blood vessels that transport blood away from heart.
· Their layer consists of three layers of tissue.
1) Tunica adventitia (Outer layer of fibrous tissue)
2) Tunica media (Middle layer of smooth muscle tissue and elastic tissue)
3) Tunica intima (Inner lining called endothelium)
Anastomoses
· Anastomoses are arteries that form a link between main arteries supplying an area;
· Example: the arterial supply to the palms of he hands and soles of the feet, the brain, the joints and to a limited extent the heart muscles.
· If one artery supplying the area is occluded, anastomotic arteries provide a collateral circulation (Alternate or backup blood vessels in the body that can take over when another artery or vein become blocked or damaged).
DISORDERS
CORONARY ARTERY DISEASE (CAD)
· CAD results from the effect of the deposition of atherosclerotic plaques in coronary arteries, which leads to reduction in blood flow to the myocardium.
· Chances of developing disease includes;
o Smoking
o High blood pressure
o Diabetes
o High cholesterol levels
o Obesity
o Family history and life style
· A progressive disorder characterized by the formation in the wall of the arteries of lesions called atherosclerotic plaques.
· The lipoprotein (phospholipid, triglycerides, and cholesterol) which are produced by the liver and intestine. There are two major lipoproteins are;
1. Low density lipoprotein (LDL)
2. High density lipoprotein (HDL)
· LDLs transport cholesterol from the liver to body cells for use in cell membrane repair and the production of steroid hormone and bile salts.
· Excessive LDLs promotes atherosclerosis.
· On the other hand, HDLs removes excess cholesterol from body cells and transport it to the liver for elimination.
Diagnosis
· Stress testing (Monitored physical stress by exercising using treadmill).
· Echocardiography (ultrasound waves to image the interior of the heart).
· Electron beam computerized tomography (which detects Ca2+ deposit in coronary arteries → indicates atherosclerosis).
· Coronary (cardiac) computed tomography radiography (in which contract medium in is injected into a vein and β-blocker is given to ↓HR.).
· Coronary angiography (it us an invasive procedure used to obtain information about the coronary arteries).
Treatment
· Antihypertensive
· Nitroglycerin
· β-blockers
· Cholesterol lowering agents
· Clots dissolving agents
· Surgery
ARRHYTHMIA
· It refers to abnormal rhythm of heart as a result of a defect in the conduction system of the heart.
· Supraventricular tachycardia (SVT) → Rapid but regular heart rate (160-200 beats/min).
· Arterial flutter → Consist of rapid, regular arterial contractions (240-360 beats/min) → AV blocked.
· Atrial fibrillation (AF) → Common arrhythmia, affecting mostly older adults. The atria may beat 300-600 beats/min.
· Ventricular tachycardia (VT) → Originates in the ventricles and is characterized by four or more ventricular premature contractions.
· Ventricles beats 120 beats/min.
CONGESTIVE HEART FAILURE (CHF)
· There is loss of pumping efficiency by the heart
· The ventricles are unable to pump blood efficiency to arterial system.
· Diagnosis: ECG, Echo, Blood test.
· Treatments:
o Ionotropic drugs
o Diuretics
o ACE inhibitor
o Vasodilators
o β-adrenergic blockers
ANGINA PECTORIS
· It is a pain syndrome due to lack of O2 supply or increase demand of O2 in the portion of the myocardium.
· The angina pectoris may cause sudden severe chest pain that may scatter o the neck, jaw, back, and arm.
· Also persist nausea, vomiting, indigestion, and diaphoresis.
Types
1. Stable angina (common form of angina → squeezing or burning feeling in the chest).
2. Unstable angina (acute coronary syndrome → required hospitalization to prevent myocardial infraction).
3. Variant angina (unpredictable pattern of angina, that occurs at rest or sleep and due to coronary spasm).
Treatment
· Nitrates
· β-blockers
· Ca2+ channel blockers
· K+ channel opener
· Ivabradine

Hi….!! My name is Smrutiranjan Dash, From Odisha, India. Professionally I am Assistant Professor at The Pharmaceutical College, Barpali, Odisha, department of Pharmacology.
