Insulin and hypoglycemic drugs
Diabetes mellitus
· It is chronic metabolic disorder characterized by a high blood glucose concentration (Hyperglycemia).
MAJOR TYPES OF DIABETES MELLITUS
Type-I diabetes | Type-II diabetes |
· Body no longer able to produce insulin. · Usually develops during childhood, but develops at any age. | · Still producing insulin, but it does not make enough. · Can develops at any age but is most common in adults over age 45. |
FACTORS | |
· Family history | · Overweight, high blood pressure etc. |
SYMPTOMS | |
· Blurry vision · Frequent urination · Increase appetite and thirst · Mood changes · Tiredness and weakness · Unexpected weight loss | · Blurry vision · Frequent urination · Increase appetite and thirst · Mood changes · Tiredness and weakness · Unexpected weight loss |
PREVENTION | |
· No known prevention methods | · Healthy lifestyle |
TREATMENT | |
· Insulin injection | · Healthy living |
HISTOLOGY
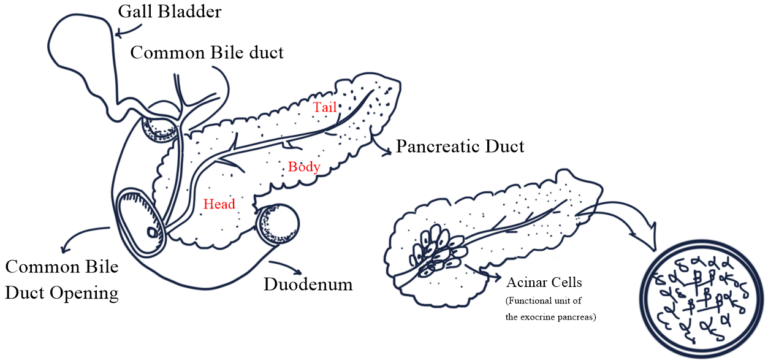
· Pancreas is the second largest gland of the human body lies in the abdomen behind the stomach and it plays an important role in maintaining sugar level.
· Pancreas has exocrine as well as endocrine function.
· Exocrine: secrete enzyme that help with digestion.
· Endocrine: hormone secreted to the blood by endocrine gland of the pancreas maintain blood glucose level.
· 99% of the pancreatic mass concerned with exocrine and about 1% mass concerned with endocrine system.
· The Acinar cell of the pancreas is the functional unit of the exocrine.
· It synthesizes, stores, and secretes digestive enzymes which are activated when it reached to the duodenum.
· The endocrine system of the pancreas composed of cluster of cells called “Islet of Langerhans”.
· Pancreatic cell basically consists of four types of cell.
o α – A cell → Glucagon producing
o β – B cell → Produce Insulin and Amylin
o δ – D cell → Produce somatostatin
o pp – F cell → Pancreatic polypeptide
INSULIN
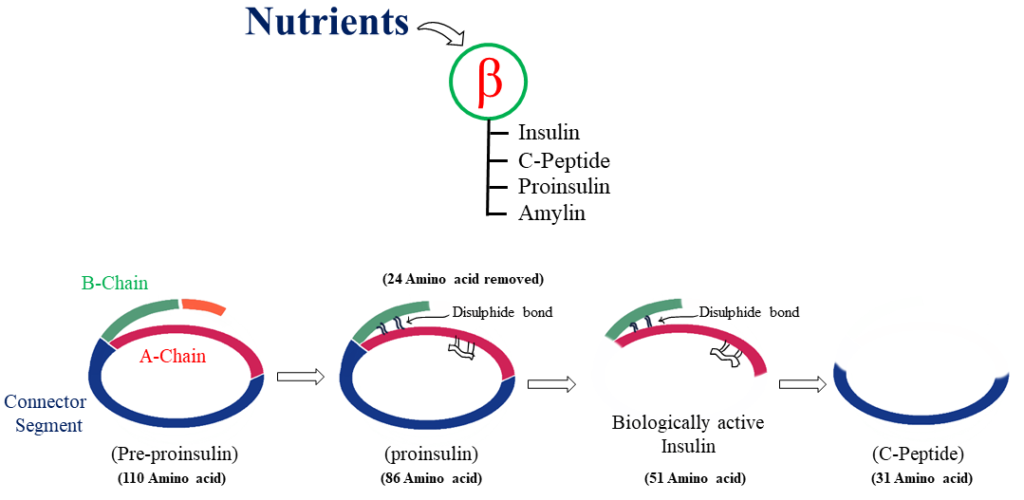
· insulin is a polypeptide hormone consisting of two peptide chains that are connected by Disulphide bonds.
· It is synthesized as a precursor (Proinsulin) that undergoes proteolytic cleavage to form insulin and C-Peptide, both of which are secreted by β-cell of the pancreas.
SYNTHESIS OF INSULIN
· The pre-proinsulin consists of 110 amino acid residues.
· After synthesized of 24 amino acid the pre-proinsulin is converted to proinsulin which is contain 86 amino acid residues.
· The proinsulin cleavage to form insulin and C-peptide that contain 51 and 31 amino acid respectively.
INSULIN SECRETION
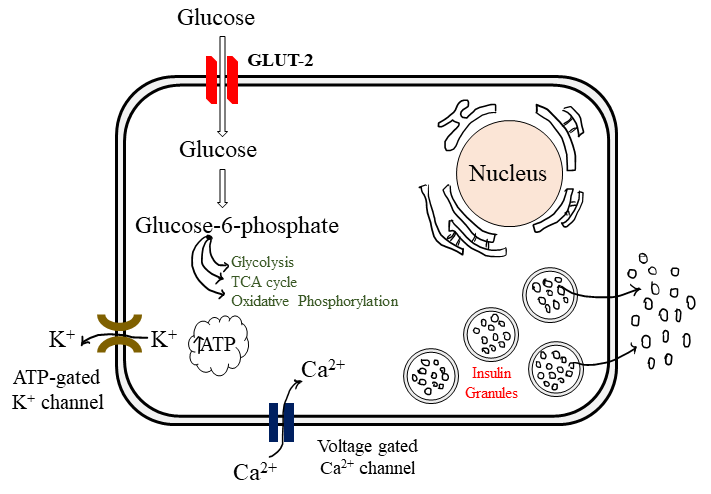
· The β-cells have a glucose sensing mechanism dependent on entry of glucose into β-cells (through GLUT-2) and its phosphorylation by glucokinase.
· Glucose entry and metabolism leads to activation of the glucosensor which indirectly inhibits the ATP sensitive K+ channel (K+ ATP) resulting partial depolarization of the β-cells.
· Increase intracellular Ca2+ availability.
· Exocytosis release of Insulin storing granules.
MECHANISM OF ACTION
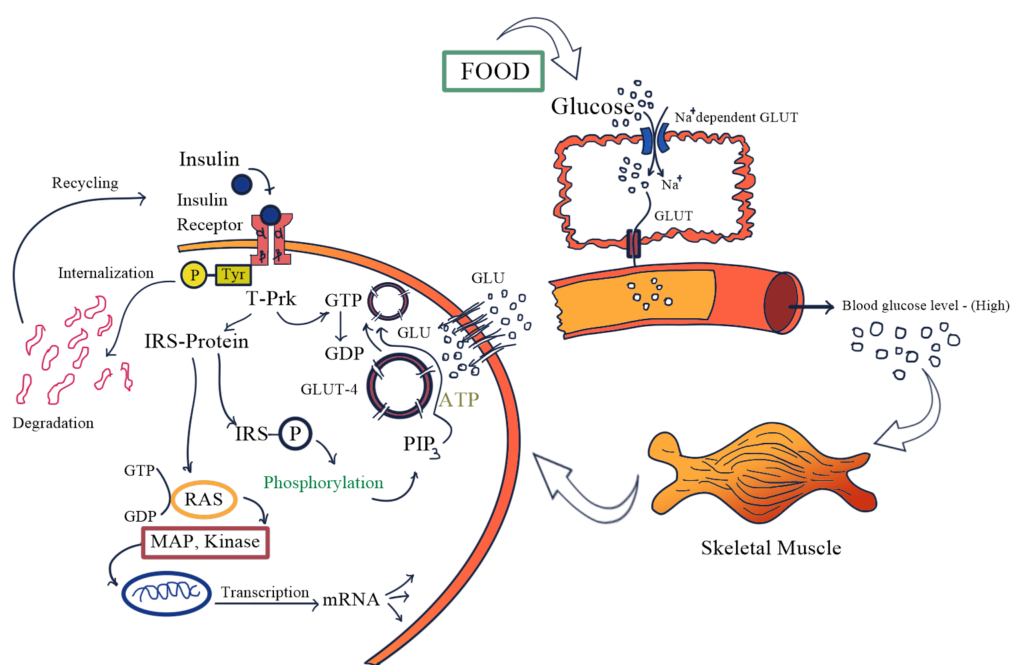
· The insulin receptor is a receptor tyrosine kinase (RTK)
· Consisting of 2α (extracellular) and 2 intracellular β sub-units linked together by Disulphide bonds.
· Insulin bind to α subunits site, while β subunit have tyrosine protein kinase activity.
· After binding of insulin to β subunits induce activation of tyrosine kinase of the β subunits.
· Phosphorylation tyrosine residues of Insulin receptor substrate protein (IRS-P).
· Phosphorylation and dephosphorylation activate the signal and results stimulation or inhibition of enzymes involved in the rapid metabolic action of insulin.
· PI3 – kinase generate PIP3 which mediate the action on metabolic action of Insulin.
· PIP3 and other tyrosine phosphorylated guanine exchange protein translocate GLUT4 from cytosol to plasma membrane, especially in skeletal muscle and adipose tissue.
FATE OF INSULIN
· It is a peptide, gets degraded in the GIT if given orally.
· Injected insulin metabolized primary in the liver and small extend in the kidney and muscles.
· Half of the Insulin enters the portal vein circulation.
· During biotransformation A and B chains of the Insulin are separated and Disulphide bonds are reduced.
· Plasm t ½ is 5-9 minutes.
ADVERSE REACTION
· Hypoglycemia
· Weight gain
· Local injection site reaction
· Lipodystrophy (Abnormal distribution of fats)
INSULIN PREPARATION
1. Rapid and short acting Insulin preparation
· Regular Insulin is a short acting, soluble, crystalline, zinc Insulin.
· Insulin lispro, Aspart, and glulisine are rapid acting Insulin.
· Peak level of Insulin lispro are 30-90 minutes.
· Rapid Insulin should be administered SC. 3 minutes before meal, whereas rapid acting Insulin are administered before 15 minutes.
2. Intermediate acting
· Neutral protamine hagedorn (NPH)
· Administered AC. → Not i.v.
3. Long acting
· The iso-electric point of insulin glargine is lower than that of human Insulin, leading to formation of precipitate at the injection site that release over an extended period.
· Slower onset of action than NPH
4. Insulin combination
· Human Insulin: 70% NPH Insulin + 30% regular Insulin OR 50% of each.

Hi….!! My name is Smrutiranjan Dash, From Odisha, India. Professionally I am Assistant Professor at The Pharmaceutical College, Barpali, Odisha, department of Pharmacology.

Im very pleased to find this site. I need to to thank you for ones time for this particularly fantastic read!! I definitely really liked every part of it and I have you bookmarked to see new information on your site.
I need to to thank you for this good read!! I certainly enjoyed every bit of it. I have you saved as a favorite to look at new things you postÖ