IMMUNOSUPPRESSANT
· Immunosuppressant are drugs that inhibit cellular or humoral or both types of immune responses.
· These drugs have met a high degree of success in organ transplant and autoimmune diseases.
Cytokine
· Cytokines are soluble, antigen-nonspecific signaling proteins that bind to cell surface receptors on a variety of cells.
· Cytokine includes interleukins (ILs), interferons (IFNs), tumor necrosis factors (TNFs), transforming growth factors, and colony-stimulating factors.
· IL-2, a growth factor that stimulates the proliferation of antigen-primed (helper) T cells, which subsequently produce more IL-2, IFN-γ, and TNF-α.
Cytokine | Action |
IL-1 | · Enhances the activity of (natural killer) NK cells. · Attracts neutrophils and macrophages. |
IL-2 | · Induces proliferation of antigen-primed T cells. · Enhances the activity of NK cells. |
IFN-γ | · Enhances the activity of macrophages and NK cells. · Increases expression of (major histocompatibility complex) MHC molecules. · Enhances the production of IgG2a. |
TNF-α | · Cytotoxic effect on tumor cells. · Induces cytokine secretion in the inflammatory response. |
Classification
1. Calcineurin inhibitors (Specific T-cell inhibitors)
· Cyclosporine (Ciclosporin), Tacrolimus
2. m-TOR inhibitors
· Sirolimus, Everolimus
3. Anti-proliferative drugs (Cytotoxic drugs)
· Azathioprine, Methotrexate, Cyclophosphamide, Chlorambucil, Mycophenolate mofetil (MMF)
4. Glucocorticoids
· Prednisolone and others
5. Biological agents
(a) TNFα inhibitors: Etanercept, Infliximab, Adalimumab
(b) IL-1 receptor antagonist: Anakinra
(c) IL-2 receptor antagonists: Daclizumab, (anti CD-25 antibodies) Basiliximab
(d) Anti CD-3 antibody: Muromonab CD3
(e) Polyclonal antibodies: Antithymocyte antibody (ATG), Rho (D) immune globulin.
Calcineurin inhibitors (Specific T-cell inhibitors)
Cyclosporine (Ciclosporin)
· Cyclosporine is a lipophilic cyclic polypeptide extracted from the soil fungus Beauveria nivea.
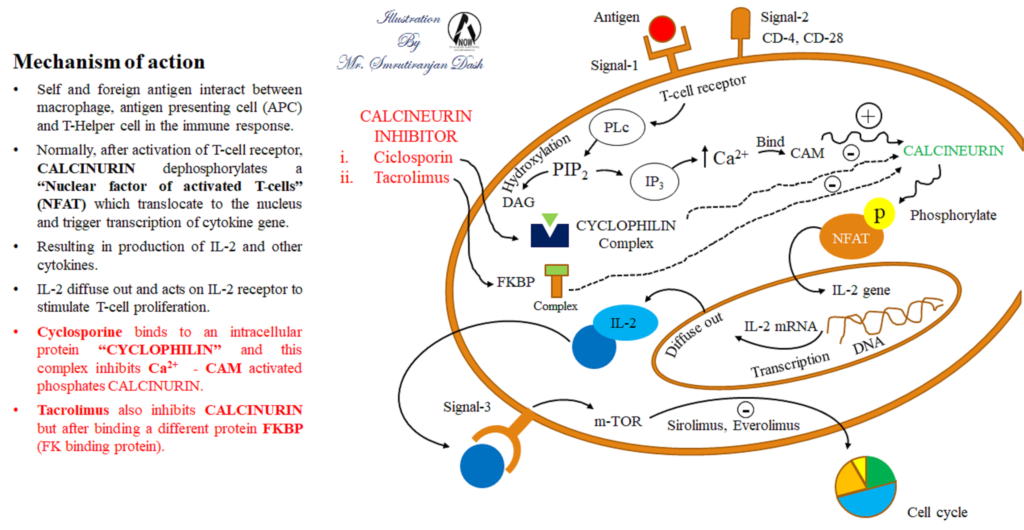
Mechanism of action
· Self and foreign antigen interact between macrophage antigen presenting cell (APC) and T-helper cell in the immune response.
· Normally, after activation through T-cell receptor, calcineurin dephosphorylates a ‘nuclear factor of activated T-cells’ (NFAT) which translocates to the nucleus and triggers transcription of cytokine genes resulting in production of IL-2 and other cytokines.
· IL-2 diffuses out and acts on IL-2 receptor to stimulate T-cell proliferation and other processes, carrying forward the immune response.
· Cyclosporine binds to an intracellular protein ‘Cyclophilin’ and this complex inhibits Ca2+-Calmodulin (Ca2+-CAM) activated phosphatase ‘Calcineurin’.
· Tacrolimus also inhibits calcineurin, but after binding to a different protein FKBP (FK binding protein).
Therapeutic uses
· Cyclosporine is used to prevent rejection of kidney, liver, and cardiac allogeneic transplants.
Pharmacokinetics
· Given orally or i.v.
· Oral absorption is variable due to metabolism by a cytochrome P450 (CYP3A4) iso-enzyme in the gastrointestinal (GI) tract and efflux by P-glycoprotein (P-gp).
· About 50% of the drug is bound to erythrocytes.
· Metabolized by liver.
· Excretion through biliary route into the feces.
Adverse effects
· Nephrotoxicity is the most common.
· Hepatotoxicity.
· Hypertension
· Hyperlipidemia
· Hyperkalemia
· Tremor
· Hirsutism
· Glucose intolerance, and gum hyperplasia.
Tacrolimus
· It is isolated from the soil fungus Streptomyces tsukubaensis.
Mechanism of action
· Tacrolimus exerts its immunosuppressive effects in the same manner as cyclosporine, except that it binds to a different immunophilin, FKBP-12 (FK-binding protein), and the complex then binds to calcineurin.
Therapeutic uses
· Preventing heart, liver, pancreas, and kidney rejections (along with glucocorticoids).
Pharmacokinetics
· Administer orally or i.v. but, as with cyclosporine oral absorption of tacrolimus is incomplete and variable
· Tacrolimus is subject to gut metabolism by CYP3A4/5 isoenzymes and is a substrate for P-gp.
· Absorption is decreased if the drug is taken with high-fat or high-carbohydrate meals.
· Drugs and metabolites are primarily eliminated in the feces.
Adverse effect
· Nephrotoxicity and neurotoxicity
· Alopecia
· Cardiovascular toxicities, such as hypertension and hyperlipidemia (lower incident).
· Other toxicities are same as cyclosporine except Hirsutism.
m-TOR inhibitors
Sirolimus (rapamycin)
· It is obtained from fermentations of the soil mold Streptomyces hygroscopicus.
Mechanism of action
· Binds to FK-binding protein as tacrolimus.
· Sirolimus binds to m-TOR (a serine/threonine kinase), interfering with signal 3.
· Binding of sirolimus to m-TOR blocks the progression of activated T cells from the G1 to the S phase of the cell cycle.
· Sirolimus does not lower IL-2 production but, rather, inhibits the cellular response to IL-2.
Therapeutic uses
· Renal transplantation
· In combination with cyclosporine and corticosteroids – lower doses and also lower toxicity.
· The combination of sirolimus and cyclosporine is synergistic because sirolimus works later in the immune activation cascade.
Pharmacokinetics
· Available as oral solution and tablet.
· Readily absorbed.
· Decrease the absorption with high fat meals.
· Half-life 57-62.
· Metabolized by the CYP3A4 iso-enzyme.
· Sirolimus also increases the concentrations of cyclosporine, and careful blood level monitoring of both agents must be done to avoid harmful drug toxicities.
Adverse effect
· Hyperlipidemia (common).
· Headache, nausea and diarrhea.
· Leukopenia, and thrombocytopenia.
Everolimus
· Another m-TOR inhibitor, is approved for use in renal transplantation. It is also indicated for second-line treatment in patients with advanced renal cell carcinoma.
Mechanism of action
· It inhibits activation of T cells by forming a complex with FKBP-12 and subsequently blocking m-TOR.
Therapeutic uses
· Used to prevent rejection in kidney transplant recipients in combination with basiliximab, cyclosporine, and corticosteroids.
Pharmacokinetics
· Rapidly absorbed, but absorption is decreased with high-fat meals.
· Short half-life, requires twice daily dosing.
· Everolimus increases drug concentrations of cyclosporine, thereby enhancing the nephrotoxic effects of cyclosporine, and is, therefore, recommended to be used with reduced doses of cyclosporine.
Adverse effects
· Similar to sirolimus.
· An additional adverse effect noted with Everolimus is angioedema.

Hi….!! My name is Smrutiranjan Dash, From Odisha, India. Professionally I am Assistant Professor at The Pharmaceutical College, Barpali, Odisha, department of Pharmacology.
