Malaria
· A disease caused by a Plasmodium parasite, transmitted by the bite of infected Anopheles mosquito.
· Malaria caused by following species of parasites
1. Plasmodium vivax
2. Plasmodium ovale
3. Plasmodium falciparum
4. Plasmodium malariae
5. Plasmodium knowlesi
· According to WHO estimation (2011) nearly 0.655 million death occur due to malaria each year globally.
Symptoms
· Headache
· Fever
· Fatigue
· Back pain
· Chills
· Dry cough
· Spleen enlargement
· Nausea and vomiting.
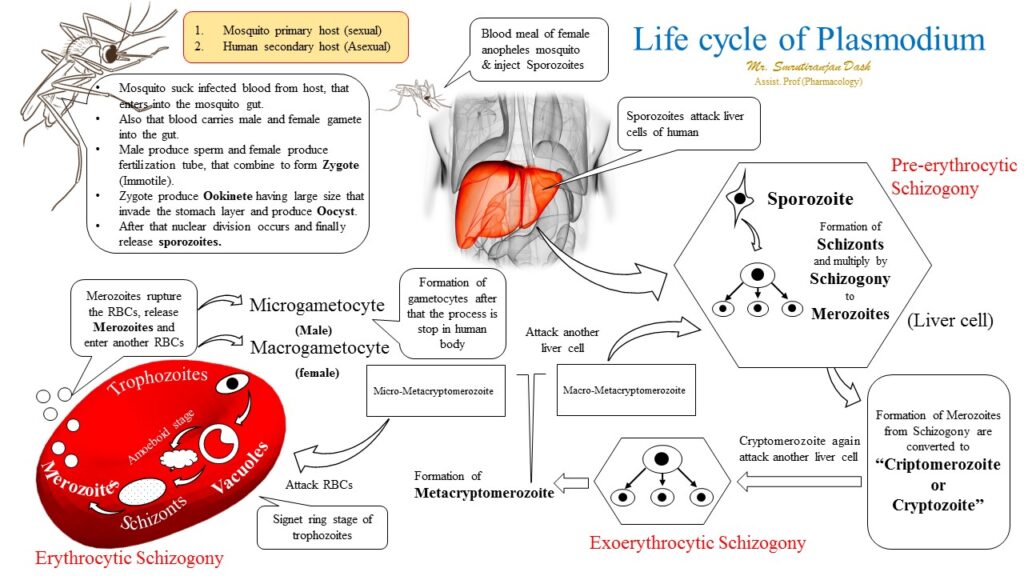
Life cycle of malaria
· The malaria parasite life cycle involves two hosts. During a blood meal, a malaria-infected female Anopheles mosquito inoculates sporozoites into the human host.
· Sporozoites infect liver cells.
· Mature into schizonts.
· Which rupture and release merozoites.
· After this initial replication in the liver, the parasites undergo asexual multiplication in the erythrocytes. Merozoites infect red blood cells.
· The ring stage trophozoites mature into schizonts, which rupture releasing merozoites.
· Some parasites differentiate into sexual erythrocytic stages (gametocytes).
· Blood stage parasites are responsible for the clinical manifestations of the disease.
· The gametocytes, male (microgametocytes) and female (macrogametocytes), are ingested by an Anopheles mosquito during a blood meal.
· The parasites multiplication in the mosquito is known as the sporogonic cycle.
· While in the mosquito’s stomach, the microgametes penetrate the macrogametes generating zygotes.
· The zygotes in turn become motile and elongated (ookinetes).
· Which invade the midgut wall of the mosquito where they develop into oocysts.
· The oocysts grow, rupture, and release sporozoites.
· Which make their way to the mosquito’s salivary glands. Inoculation of the sporozoites into a new human host perpetuates the malaria life cycle.
· Only female mosquitoes feed on blood, male mosquitoes feed on plant nectar, and do not transmit the disease.
· Malaria parasites can also be transmitted by blood transfusions, although this is rare.
Classification
1. 4-aminoquinolines
e.g. chloroquine, hydrochloroquine, amodiaquine, pyronaridine.
2. 8-aminoquinolines
e.g. primaquine, tefenoquine, Bulaquine.
3. Cinchona alkaloids
e.g. Quinine, Quinidine.
4. Quinolone methanol
e.g. Mefloquine.
5. Biguanides
e.g. Proguanil, Chlorproguanil.
6. Diaminopyrimidines
e.g. Pyrimethamine
7. Sulfonamide
e.g. Sulfadoxine, Dapsone.
8. Tetracyclines
e.g. Tetracycline, Doxycycline
9. Napthoquinone
e.g. atovaquinone
10. Sesquiterpine lactones
e.g. Artesunate, Atemether, arteether,
11. Amino alcohol
e.g. Halofantrine, Lumefantrine
12. Mannish base
e.g. Pyronaridine
Therapeutic classification
1. Causal prophylaxis (primary tissue schizonticides)
· Destroy parasite in liver cells ad prevent invasion of erythrocytes.
· Example: Primaquine, Proguanil.
2. Suppressive prophylaxis
· Suppress the erythrocytic phase and thus attack of malarial fever can be used as prophylactics.
· Example: Chloroquine, Proguanil, Mefloquine, Doxycycline
3. Clinical cure (erythrocytic schizonticides)
· Used to terminate an episode of malarial fever.
4. Fast acting high efficacy
· Chloroquine, Quinine, Mefloquine, Atovaquine, Artemisin.
5. Slow acting low efficacy drugs
· Proguanil, Pyrimethamine, Sulfonamides, Tetracycline.
6. Radical curative
· Eradicate all form of p. vivax and p. oval from the body.
· Suppressive drugs + hypnozoitocidal drugs.
· For vivax: Primaquine 15 mg daily for 14 days.
7. Gametocidal
· Destroy gametocytes and prevent transmission.
· Primaquine, Artemisin (against all plasmodia)
· Chloroquine, Quinine (P. Vivax)
· Proguanil, Pyrimethamine (prevent development of sporozoites)
Chloroquine
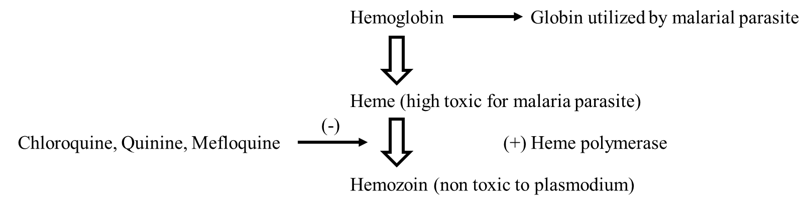
Mechanism of action
Pharmacological action
1. Antimalarial activity
· High against erythrocytic forms of vivax, ovale, malarise and sensitive strains of falciparum.
· Gametocytes of vivax
· No activity against tissue schizonts.
· Resistance develops due to efflux mechanism
2. Other parasitic infections
· Giardiasis, taeniasis, extraintestinal amoebiasis.
3. Other action
· Depressant action on myocardium
· direct relaxant effect on vascular smooth muscle
· anti-inflammatory
· antihistaminic
· local anesthesia
Pharmacokinetics
· well absorbed orally
· tmax 2-3 hours, 60% protein bound
· Concentrated in liver, spleen, kidney, lungs, and leukocytes.
· Selective accumulation in retina: ocular toxicity.
· T ½ : 3-10 days increases from few days to weeks.
Adverse effects
· Tolerance
o Nausea, vomiting, anorexia (an abnormally low body weight / fear of gaining weight).
o Skin rashes, angioneurotic edema (swelling may occur in the face, tongue, larynx, abdomen, or arms and legs.), dermatitis.
o Photosensitivity, pigmentation, exfoliative (severe inflammation of the entire skin surface).
o Long term therapy may cause bleaching of hair.
o Rarely thrombocytopenia (low platelet level), agranulocytosis (low WBC counts), pancytopenia.
· Ocular toxicity
o Temporary loss of accommodation.
o Lenticular opacities (produces swelling and opacity of the entire lens)
o Sub capsular contract (reduce vision in bright light / interfere with reading vision)
o Blue black pigmentation
o Constrictcted field of vision
· CNS
o Insomnia (poor sleeping habits)
o Transient depression seizures
o Rarely neuropathy and ototoxicity
· CVS
o ST and T wave abnormalities, decrease in BP and cardiac arrest in children reported.
Dosage
· 600 mg of base start
· 300 mg base after 8 hours
· 150 mg base BD for 2 days
· 200 mg oral tablet of chloroquine phosphate
Hydroxycloroquine
· Less toxic
· Properties and uses same as chloroquine.
Amodiaquine
· As effective as chlroquine.
· Similar pharmacological action.
· Chloroquine resistant strains may be effective.
· Adverse effect: headache, photosensitivity, agranulocytosis (rare).
· Amodiaquine is not recommended for prophylaxis treatment.
Quinine
· It is isolated form the bark of cinchona (1820 Pelletier and caventou).
· Same mechanism of action to chloroquine.
Pharmacological action
1. Antimalarial action
· Erythrocytic, forms of all malarial parasites including resistant falciparum strain.
2. Local irritant effect
· Local pain sterile abcess.
3. Cardiovascular
· Depress myocardium: decrease excitability, decrease conductivity, increase refractory period.
4. Miscellaneous action
· Mild analgesic antipyretic activity, stimulation of uterine smooth muscle, curaremimitic effect.
Adverse drug reaction
· Tinnitus, nausea, and vomiting.
· Headache mental confusion, vertigo, difficulty in hearing and visual disturbances.
· Diarrhea, flushing and marked perspiration.
· High doses: delirium, fever, tachypnea, respiratory depression, cyanosis.
· Idiosyncrasy: similar to cinchonism but occurs in therapeutic doses.
· Cardiovascular toxicity: cardiac arrest, hypotension, fatal arrhythmias.
· Black water fever (massive intravascular hemolysis).
· Hypoglycemia.
Uses
· Uncomplicated resistant falciparum malaria
PRIMAQUINE
· Poor erythrocytic schizonticides
· Has marked effect on primary and secondary hepatic phases of malarial parasite
· Highly active against gametocytes and hypnozoites.
Mechanism of action
· Intermediate act as oxidant that are responsible for the schizontocial action
Pharmacokinetics
· Readily absorbed after oral absorption
· Oxidized in liver with a plasma half-life of 3-6 hours
· Excreted in urine within 24 hour
· Not a cumulative drug.
Adverse effects
· Abdominal pain, gastrointestinal upset, weakness or uneasiness chest
· Leucopenia (high dose) (reduced number of white blood cells)
· Hemolysis
· Methaemoglobinaemia
· Tachypnoea (abnormally rapid breathing).
· Cyanosis (bluish discoloration – especially skin and mucous membrane, due to excessive concentration of deoxyhemoglobin in the blood caused by deoxygenation).
Contraindications
· Should not be given during pregnancy because fetus is glucose-6-phosphate dehydrogenase ( G 6-PD) deficient
Clinical uses
· Radical cure of relapsing malaria (P.ovale and P.vivax)
· Single 45mg dose given with curative dose of chloroquine to kill gametes (P. falciparum)
MEFLOQUINE (MQ)
· Fast acting erythrocytic (blood) schizontocide but slower than CQ or quinine.
· Effective against CQ-sensitive as well as resistant Plasmodia.
· Efficacious suppressive prophylactic for multi-resistant P. falciparum.
Mechanism of action
· It accumulates in infected RBCs, binds to heme and this complex damages the parasite’s membrane.
· Action at parasitic cytosol rather than in the acidic vacuole.
Pharmacokinetics
· Prolonged absorption after oral ingestion
· It is highly plasma protein bound and concentrated in the liver, lung and intestines
· Extensive metabolism occurs in liver and is primarily secreted in bile
· It has a long half-life (17days) due to its concentration in various tissues and its continuous circulation through the enterohepatic and enterogastric systems
· Its major excretory route is feces.
Adverse effects
· MQ is bitter in taste
· At high doses:
o Nausea, vomiting, diarrhea, abdominal pain, bradycardia
o Ataxia, hallucinations, depression
· MQ is safe in pregnancy
· Rare events of toxicity are seen.
Contraindications
· In patients with anxiety, depression, psychosis, and in cardiac conduction defects
Drug interactions
· Cardiac arrests are possible if MQ is taken concurrently with quinine or quinidine
Uses
· Effective for multidrug resistant P. falciparum
· However its use is restricted due to its toxicity, cost and long half life

Hi….!! My name is Smrutiranjan Dash, From Odisha, India. Professionally I am Assistant Professor at The Pharmaceutical College, Barpali, Odisha, department of Pharmacology.
