Coronary artery disease is the most common heart disease and most common cause of death worldwide. According to WHO 3-7 million people die from coronary artery disease every year. An estimated data that CAD is responsible for about 10% disability-adjusted life years in low income countries and 18% in high income countries. The most common disease associated with CAD is Angina Pectoris.
Angina Pectoris
The angina pectoris is a pain syndrome due to lack of oxygen supply or increase demand of oxygen in portion of the myocardium. The angina pectoris may cause sudden, severe chest pain that may scatter to the neck, jaw, back and arms. Also persist, nausea, vomiting, indigestion and diaphoresis.
Types of angina
1) Stable / Classic / Typical Angina
2) Unstable Angina
3) Prinzmetal / Variant / rest Angina
Stable Angina
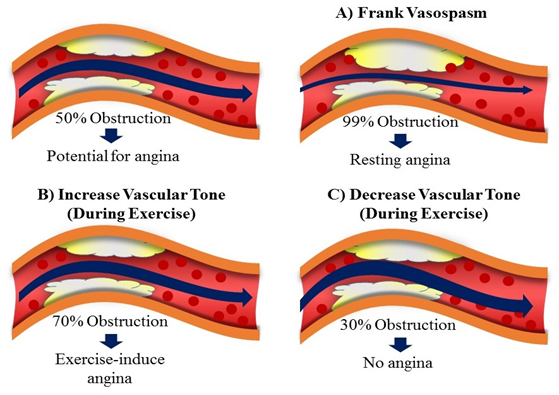
Stable angina is the most common form of angina and it is usually characterized by short squeezing or burning feeling in the chest. Some “atypical” condition with extreme fatigue, sweeting and nausea. The typical conditions are more common in women, diabetic patient and old age. Basically the stable angina occurs due to obstruction of artery produced by atherosclerosis, so that the coronary perfusion is reduced.
Unstable Angina
Unstable angina is the form of acute coronary syndrome and requires hospitalization to prevent progression of myocardial infraction (MI) and death. The severity is most due to rupture of atheromatous plaque attracting platelet disposition and progressive occlusion of coronary artery.
Prinzmetal / Variant / Rest / Vasospastic Angina
Prinzmetal angina is an unpredictable pattern of angina that occurs at rest or sleep and is due to coronary spasm. In this case decrease blood flow to the heart muscle from the spasm of the coronary artery.
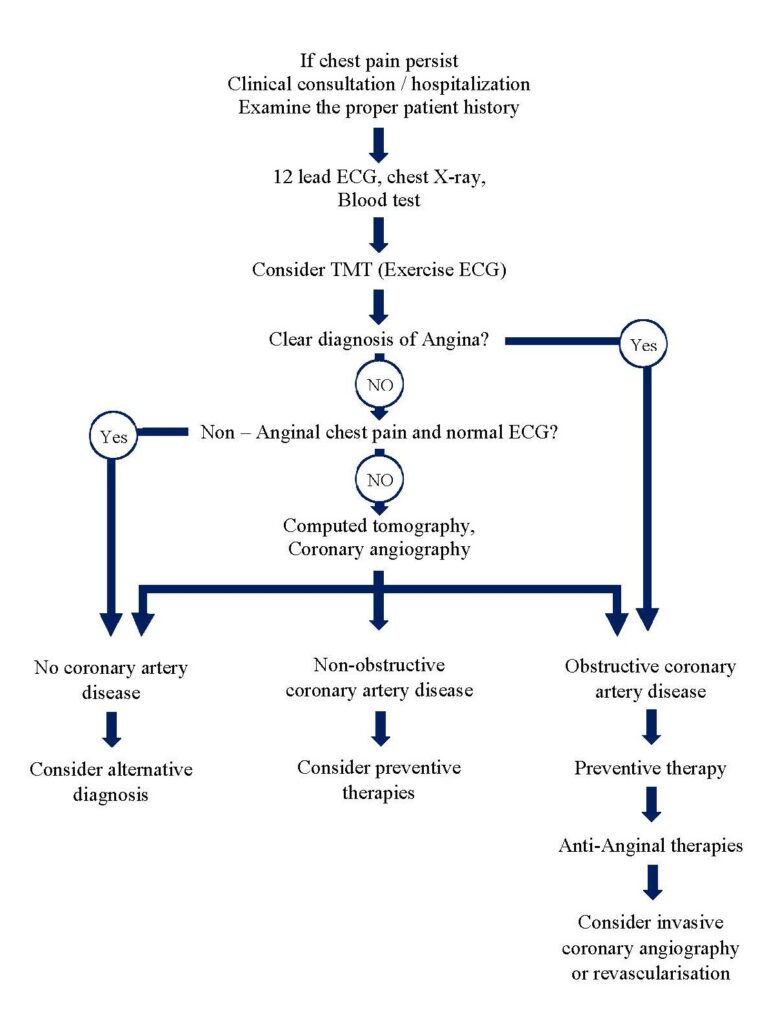
Clinical diagnosis
· Stable angina is characterised by central chest pain, discomfort or breathlessness.
· Stress testing
· Exercise ECG (TMT) planar or down sloping ST segment depression of 1mm or more in indicative of ischaemia. Up sloping ST depression in less specific (False positive results).
· Echocardiogram (Echo)
· Angiography
Management
· Life style management.
· Anxiety and misconception should be prohibited.
· Proper education.
· Cessation of smoking.
· Identification of risk factor.
Proper medication therapy.
· Patients with angina secondary to CAD should receive antiplatelet therapy.
· Low dose of Aspirin (75mg).
· Clopidodrel (75mg / day) in an equally effective alternative if Aspirin cause dyspepsia or other side effects.
· Consider station, even cholesterol level is normal.
Statin (HMG-COA reductase)
It is a class of drugs that lowers the level of cholesterol, in the body by decreasing the production of cholesterol in liver. Statin blocks the enzyme hydroxyl methyalglutaryl coenzyme A reductase (HMG-COA reductase). Some example of statin are as follows:
· Atorvastatin (Lipitor)
· Fluvastatin (Lescol, Lescol XL)
· Levastatin (Mevacor, Altoprev)
· Pravastatin (Pravachol)
· Rosuvastatin (Crestor)
· Simvastatin (Zocor)
· Pistavastatin (Livala)
Anti-Anginal drug therapies
1. Nitrates
a) Short acting: Glyceryl Nitrate (GTN, Nitrogycerin)
b) Long acting: Isosorbide dinitrate (short acting by sublingual route), Isosorbide mononitrate, Erythrityl tetra nitrate, Pentaerythritol trinitrate.
2. β – Blockers: Propranolol, Metoprolol, Atenolol and others.
3. Calcium channel blockers:
a) Phenyl alkylamine: Verapamil
b) Benzothiazepine: Diltiazem
c) Dihydropyridine: Nefidipine, Felodipine, Amlodipine, Nitrendipine, Nimodipine, Lacidipine, Lercaniipine, Benidipine.
4. Potassium channel opener: Nicorandil.
5. Others: Dipyridamole, Trimetazidine, Ranolazine, Ivabradine, Oxyphedrine.
Nitrates
GTN has the short duration of action therapies, when it administered in sublingual route. GTN administered metered-dose aerosol (400µg/day) or as a tablet (300 or500 µg) is usually relieve an attack in 2-3 minutes.
· GTN transcutaneous (5-10 daily)
· Slow release buccal tablet (1-5 four times daily)
· Isosorbide dinitrate (10-20mg 3 times daily)
· Isosorbide mononitrate (20-60mg once / twice daily)
Continuous therapy of Nitrates can cause pharmacological tolerance, but this can be avoided by 6-8 hours nitrate free period.
Duration of action of Nitrates
Preparation | Peak action | Duration of action |
Sublingual GTN (0.5mg) | 4-8mins | 10-30mins |
Buccal GTN | 4-10mins | 30-300mins |
Transdermal GTN | 1-3hrs | Up to 24hrs |
Oral Isosorbide dinitrate (5-10mg Sublingual, 10-20mg Oral) | 45-120mins | 20-40mins 2-6hrs |
Oral Isosorbide Mononitrate (20-40 oral) | 45-120mins | 6-10hrs |
Erythrityl tetranitrate (5-15mg tablet) |
| 3-6hrs |
Pentaerythritol tetranitrate (0mg tablet, 80mg SR tablet) |
| 3-5hrs 8-12hrs |
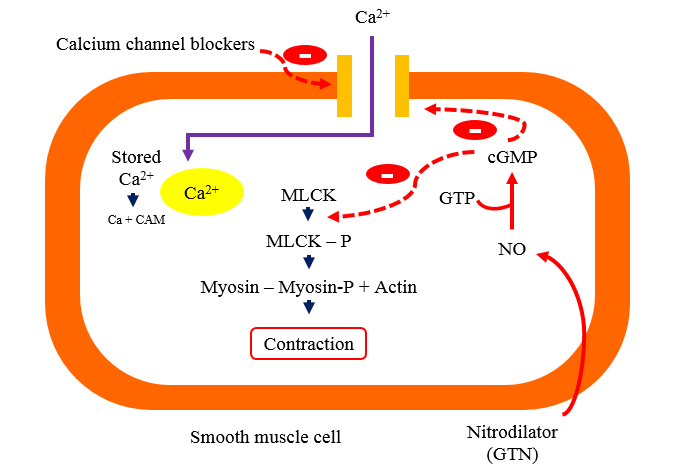
Mechanism action of Nitrates
· Organic Nitrates are metabolised or denitrated enzymatically in smooth muscle cells to release the reactive free radical Nitric oxide (NO).
· Which increases the cytosolic guanylyl cyclase, thus increase the cGMP (Cyclic guanosine monophosphate) that causes dephosphorylation of myosin light chain kinase (MLCK) through a cGMP dependent protein kinase.
· Reduce availability of phosphorylated (active) MLCK interfere with Actin to cause contraction consequently relaxation occurs.
· Raised intracellular cGMP may also reduce Ca2+ entry contributing to relaxation.
Pharmacokinetics
Organic nitrates are lipid soluble. Well absorbed from, buccal mucosa, intestine and skin. Isosorbide dinitrate undergo extensive and variable first pass metabolism in liver. The partly metabolites (denitrated by a glutathione reductase and a mitochondrial aldehyde dehydrogenase) are less active, but longer .
Adverse effect
Headache, tolerance develops on continued use. Flushing, weakness, sweating, palpitation, dizziness and fainting. Methamoglobinemia, rashes are rare (mostly with pentaerythritol tetranitrate).
Tolerance
Generally long acting or sustain acting preparation produced tolerance. The mechanism of tolerance is not understood, but it happened due to reduce ability to generate NO. For prevention of tolerance provide the bitrates free interval every day.
Interaction
Sildenafil cause severe hypotension, MI and death.
Drug class | Adverse effect | Drug interaction | Instruction |
β-blocker. · Atenolol · Metoprolol · Propranolol | · Bradycardia worsening · peripheral vascular disease, · fatigue · sleep disturbance · depression · blunt hypoglycaemia awareness · asthma | β2 agonists (blunted effect); nondihydropyridine calcium-channel blockers (additive effects) | · β1-selective agents preferred · (Atenolol, metoprolol). |
Dihydropyridine calcium channel Blockers. · amlodipine · felodipine · nifedipine | · Peripheral edema · headache · Fushing · rebound tachycardia (immediate release formulations) · hypotension | CYP 3A4 substrates (will increase drug concentrations) | · Avoid short-acting agents as they can worsen angina. |
Non dihydropyridine calcium channel Blockers. · diltiazem · verapamil | · Bradycardia · Constipation · Heart failure · Gingival hyperplasia (verapamil) · Edema (diltiazem) | CYP 3A4 substrates (will increase drug concentrations); increase digoxin levels; β blockers and other drugs affecting AV node conduction (additive effects) | · Avoid in patients with heart failure |
Organic nitrates · isosorbide dinitrate · isosorbide mononitrate · nitroglycerin | · Headache · Hypotension · Flushing · tachycardia | Contraindicated with PDE5 inhibitors (sildenafil and others) | · Ensure nitrate-free interval to prevent tolerance |
Sodium-channel inhibitor · ranolazine | · Constipation, headache, edema, dizziness, QT interval prolongation | Avoid use with CYP 3A4 inducers (phenytoin, carbamazepine, St. John’s wort) and strong inhibitors (clarithromycin, azole antifungals) and agents that prolong QT interval (citalopram, quetiapine, others) | · No effect on hemodynamic parameters |

Hi….!! My name is Smrutiranjan Dash, From Odisha, India. Professionally I am Assistant Professor at The Pharmaceutical College, Barpali, Odisha, department of Pharmacology.

canadian drugs pharmacy canada pharmaceuticals online
canadian pharmacy generic viagra online pharmacies
canadian pharmacy king https://disvaiza.mystrikingly.com/