Adrenergic Antagonist
· These are drugs which antagonize the receptor action of adrenaline and related drugs. They are competitive antagonists at α or β or both α and β adrenergic receptors.
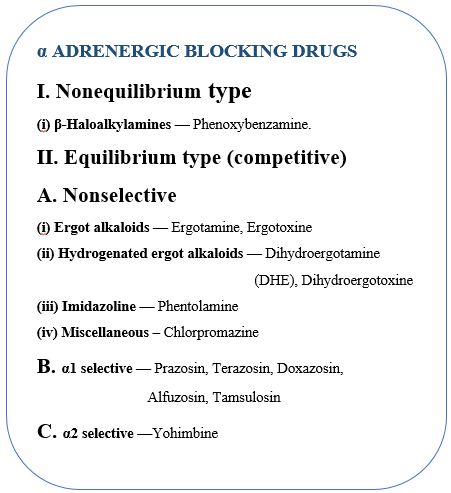
α-ADRENERGIC BLOCKING AGENTS
· These drugs inhibit adrenergic responses mediated through the α adrenergic receptors without affecting those mediated through β receptors.
· Blockade of these receptors reduces the sympathetic tone of the blood vessels, resulting in decreased peripheral vascular resistance.
Phenoxybenzamine
· covalently to both α1 and α2 receptors.
· The block is irreversible and noncompetitive, and the only way the body can overcome the block is to synthesize new adrenoceptors.
· Time period for newly synthesized adrenoreceptors required a day or longer.
Action
Cardiovascular Effects
· Prevents vasoconstriction of peripheral blood vessels.
· The decreased peripheral resistance provokes a reflex tachycardia.
· Blocking presynaptic inhibitory α2 receptors in the heart, results in more norepinephrine release, which stimulates β1 receptors on the heart, increasing cardiac output.
· So, this drug has been unsuccessful in maintaining in blood pressure.
CNS
· stimulation, nausea and vomiting on rapid i.v. injection. However, oral doses produce depression, tiredness and lethargy.
Major side
· postural hypotension
· Palpitation
· Nasal blockage
· Miosis
Therapeutic Uses
· Pheochromocytoma (a catecholamine-secreting tumor of cells derived from the adrenal medulla).
· surgical removal of the tumor to prevent a hypertensive crisis, and it is also useful in the chronic management of inoperable tumors.
· Raynaud disease (The fingers, toes, ears and tip of the nose are commonly involved and feel numb and cool in response to cold temperatures or stress.)
· Frostbite (an injury caused by freezing of the skin and underlying tissues).
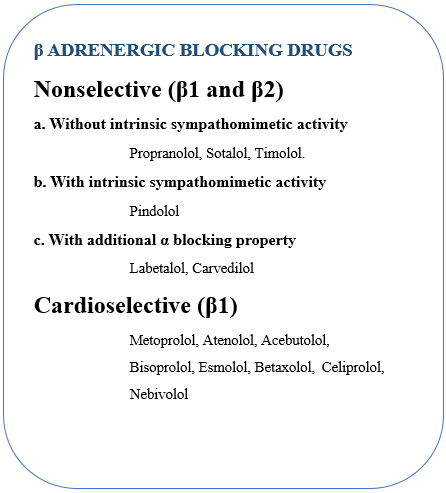
β-ADRENERGIC BLOCKING AGENTS
· Nonselective β-blockers act at both β1 and β2 receptors.
· β-Blockers are effective in treating
o hypertension,
o angina,
o cardiac arrhythmias,
o myocardial infarction,
o heart failure,
o hyperthyroidism, and glaucoma.
o They are also used for the
o prophylaxis of migraine headaches.
PROPRANOLOL
· Blocks both β1 and β2 receptors with equal affinity.
Cardiovascular
· Propranolol diminishes cardiac output, having both negative inotropic and chronotropic effects.
· It directly depresses sinoatrial and atrioventricular nodal activity resulting bradycardia.
· During exercise or stress, when the sympathetic nervous system is activated, β-blockers attenuate the expected increase in heart rate. Cardiac output, workload, and oxygen consumption are decreased by blockade of β1 receptors, and these effects are useful in the treatment of angina.
Blood Pressure
· No direct action on blood pressure.
· Reversal vasomotor activity
· Fall in BP by isoprenaline and rise in BP by Adrenaline.
· Increase in ERP and decrease in CO – but negligible change in BP.
· Decrease Renin release.
Respiratory
· Bronchoconstriction due to blockade of beta-2 receptors – Avoid incase of Asthma.
CNS
· No central effects are produced.
· However,
· Behavioral changes,
· Forgetfulness,
· Increased dreaming and
· Nightmares have been reported with long-term use of relatively high doses.
Local anaesthetic
· Propranolol is as potent a local anaesthetic as lidocaine, but is not clinically used for this purpose because it causes irritation at the injected site.
Skeletal Muscle
· Reduce tremor
· Reduction of exercise capacity
· Reduction of blood flow glycogenolysis and lipolysis.
Eye
· Decrease IOP by reducing production of aqueous humor glaucoma.
Pharmacokinetics:
· After oral administration, propranolol is almost absorbed.
· It is subject to first-pass effect, and only about 25% of an administered dose reaches the circulation.
· The volume of distribution of propranolol is quite large (4 L/kg), and the drug readily crosses the blood–brain barrier due to its high lipophilicity.
· Propranolol is extensively metabolized, and most metabolites are excreted in the urine.
Therapeutic Uses
· Hypertension
· Myocardial Infraction
· Angina
· Migraine
· Hyperthyroidism
Adverse Effects
· Bronchoconstriction
· Arrhythmia
· Metabolic disturbance
· CNS effects
o Including depression, dizziness, lethargy, fatigue, weakness, visual disturbances, hallucinations, short-term memory loss, emotional lability, vivid dreams.
Drug Interactions
· Drugs that interfere with, or inhibit, the metabolism of propranolol, such as cimetidine, fluoxetine, paroxetine, and ritonavir, may potentiate its antihypertensive effects. Conversely, those that stimulate or induce its metabolism, such as barbiturates, phenytoin, and rifampin, can decrease its effects.

Hi…!! This is Smrutiranjan Dash, Assistant Professor of Pharmacology from Odisha, India. With a passion for teaching and a dedication to advancing the field of pharmacology, I am committed to sharing knowledge, fostering innovation, and inspiring future healthcare professionals.
