A disorder in which the heart loses its ability to pump blood efficiently throughout the body.
Sign and symptoms
· Dilate pupils
· Skin becomes pale, gray colour
· Can’t breathe unless sitting up
· Cough
· Decrease BP
· Nausea and vomiting
· Edema
· Anxiety
· Failing oxygen saturation
· Fatigue
· Decrease urine output.
Diagnosis
· Hysical examination
· Chest X-ray
· Blood test
· Echo
· Angiogram (X-ray inside of the blood vessels)
Treatments
· The therapeutic goal for CHF is to increase cardiac output, reduce preload and after load and to increase myocardial contractility.
o Inotropic agents – increase contraction of cardiac muscle.
o PDE inhibitor (Phosphodiesterase inhibitor) – agents that increase cAMP to induce systoles and vasodilation.
o β-adrenergic agonist
o β-adrenergic antagonist
o vasodilators: calcium channel blockers
o Decrease Renin Angiotensin System activity. ACE inhibitor and AT1 antagonist.
o Diuretics agents.
Classification
1. Inotropic drugs
a. Cardiac glycosides: Digoxin, Digitoxin, Ouabain
b. Sympathomimetic: Dopamine, Dobutamine
c. Phosphodiesterase III inhibitors: Amrinone
2. Diuretics
a. High ceiling diuretics: Furosemide, Bumetanide
b. Thiazide like diuretics: Hydrochlorothiazide, Metolazone, Xipamide
3. Aldosterone antagonists
Spironolactone, Eplerenone
4. RAS inhibitors
a. ACE inhibitor: Enalapril, Ramipril
b. Angiotensin antagonist: Losartan
5. Vasodilators
a. Venodilation: Glyceryl Nitrate (GTN)
b. Arteriolar dilator: Hydralazine
c. Arteriolar – venodilator: Sod. Nitroprusside
6. β-adrenergic blockers
Metoprolol, Carvidilol, Bisoprolol
7. Others
a. Cardioprotective: Trimetazidine
b. Calcium sensitizer: Levosiendan
Cardiac Glycoside
These are the class of drugs having cardiac ionotropic effect. It increases the cardiac contractility of cardiac muscle. Cardiac glycoside found in the plant like Digitalis lanata (Digoxin), Digitalis purpurea (Digitoxin) Strophanthus gratus (Ouabain) etc. and also found in toad skin (Bufotoxin).
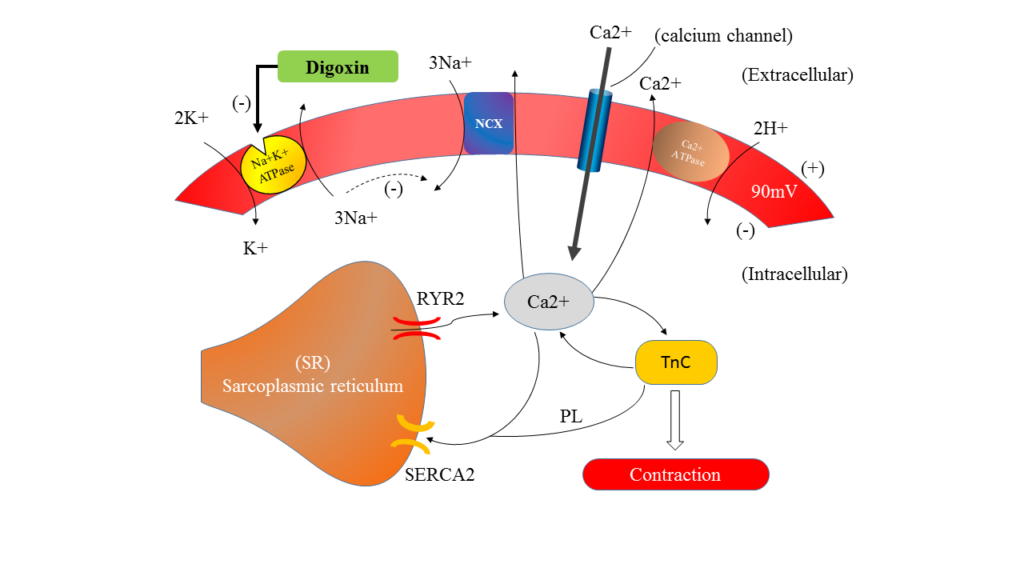
Mechanism of action
General contraction
· During depolarization (entry of Na+ and out flow of K+) Ca2+ ions enter the cell through voltage sensitive L type Ca2+ channels (> 1 nM to <100 nM during diastole).
· This Ca2+ triggers sarcoplasmic reticulum (SR) to release their stored Ca2+ through Ryanodine calcium channel 2 (RYR2), now increase cytosolic calcium concentration (about 500 nM). It trigger by activating Troponin C and promote to contraction.
· The sarcoplasmic-endoplasmic reticular calcium ATPase 2 (SERCA2) is then activated which pumps Ca2+ back into the SR (same amount that released form SR).
· Ca2+ which entered form outside during depolarization is push back to outside by sodium calcium exchange (NCX-antiporter). 3 Na+ enter and 1 Ca2+ remove from cell.
Action of Digoxin
· Digoxin is selectively bind to Na+K+ATPase of myocardial fibres and inhibit their action, hence indirectly inactive NCX.
· Na+ accumulation is gradually increase in intracellular. This results increase accumulation of Ca+ in intracellular, stored by SR.
· Due to slow biding of digoxin with Na+K+ATPase takes some time to develop muscle contraction, even after i.v. administration.
Pharmacological actions
1) On heart (Digitalis)
· Direct action on myocardial fibres and contractility properties.
· Force of contraction: due to positive ionotropic effect, increase in force of contraction with increase in dose. This is generally seen in failing heart. Systolic pressure is less and Diastolic pressure is prolong.
· Heart rate is decrease hence bradycardia is marked in CHF patients.
· Vagal tone is increased reflexly by sensitization of baroreceptors, as well as by stimulation of vagal centre.
· a) Action potential: Resting membrane potential is decrease with increase in dose. Phase ‘0’ depolarization is reduced, so Na+ channel is inactivated. This action is marked in A-V node and bundle of his. Increase phase ‘4’ depolarization in the Purkinje fibre.
· b) Effective refractory period: atrium – decrease vagal action (10th cranial nerve), increase in direct action. Ventricle – ERP is abbreviated by direct action. A-V node and bundle of his – directly increased.
· c) ECG: decrease amplitude of ‘T’ wave, increase P-R interval (at toxic dose), and shortening of Q-T interval. Depression of S-T segment (at high doses).
2) Blood vessel
· Digitalis has mild direct vasoconstriction action.
· In CHF patient: no prominent effect on BP, systolic BP may increase and diastolic BP may decrease, pulse pressure increase.
3) Kidney
· Diuresis seen in CHF patients, salt and water is gradually excreted.
4) CNS
· In higher dose activates the CTZ (chemoreceptor trigger zone) and that cause nausea and vomiting, hyperpnoea (faster breathing), central sympathetic stimulation, mental confusion, disorientation and visual disturbances.
Pharmacokinetics
· Digoxin tablet widely distributed.
· It is concentrated in heart, liver, skeletal muscle and kidney.
· Excreted by kidney.
· Oral absorption – 60-80%
· Plasma protein binding – 25%
· Onset of action – 15-30min.
· Peak time – 2-5hrs.
· Duration of action – 2-6 days.
· Plasma t ½ – 40hrs.
· Therapeutic concentration – 0.5–1.4 ng/ml.
· Toxic concentration – > 2 ng/ml.
· Daily maintenance dose – 0.125–0.5 mg.
· Daily elimination – 35%.
· Route of elimination – Renal
· Route of administration – Oral / i.v.
Doses
· DIGOXIN 0.25 mg tab., 0.05 mg/ml pediatric elixir, 0.5 mg/2 ml inj.
Adverse effect
· Anorexia, nausea, vomiting and abdominal pain.
· Gastric irritation, mesenteric vasoconstriction and CTZ stimulation.
· Fatigue, malaise, headache, mental confusion, restlessness, hyperapnoea, disorientation, psychosis and visual disturbances.
· Skin rashes and gynaecomastia are rare.
· Almost all types of cardiac arrhythmias are reported.
Adverse effect treatment
· If toxicity persist then stopped digoxin immediately.
· For tachyarrhythmias: infuse KCl 20 m.mol/hour (max. 100 m. mol) i.v. or give orally in milder cases.
· For ventricular arrhythmias: to suppress the excessive automaticity Lidocaine i.v. is the choice of drug.
· For supraventricular arrhythmias: in case of urgency propranolol i.v. may be given.
· For A-V block and bradycardia: atropine 0.6 to 1.2mg i.m. otherwise consider cardiac pacing.
Precautions and contraindications
· Hypokalemia: enhances digitalis toxicity.
· Elderly, renal or severe hepatic disease: patients are more susceptible to digoxin toxicity.
· Myocardial ischaemia: severe arrhythmias.
· Thyrotoxicosis: patients are more prone to develop digitalis arrhythmias.
· Myxoedema: these patients eliminate digoxin more slowly; cumulative toxicity can occur.
· Ventricular tachycardia: digitalis is contraindicated because it may precipitate ventricular fibrillation.
· Partial A-V block: may be converted to complete A-V block by digoxin.
· Wolff-Parkinson-White syndrome: Digitalis is contraindicated because it decreases the ERP.
Interaction
· Calcium: synergises with digitalis, precipitates toxicity.
· Quinidine: reduces binding of digoxin to tissue proteins, inhibiting renal and biliary clearance. Toxicity occur.
· Verapamil, diltiazem, captopril, propafenone and amiodarone increase plasma concentration of digoxin.
· Adrenergic drugs: can induce arrhythmias.
· Metoclopramide, sucralfate, antacids, neomycin, and sulfasalazine may reduce digoxin absorption.
· Propranolol, verapamil, diltiazem and disopyramide: may additively depress A-V conduction.
· Succinylcholine: can induce arrhythmias.
Uses
· Congestive heart failure
· Cardiac arrhythmias: Atrial fibrillation (AF), Atrial flutter (AFI), Paroxysmal supraventricular tachycardia (PSVT).
A, B, C, D, E heart failure treatment
A. Angiotensin converting enzyme inhibitors, Anticoagulants, Amiodarone, AICD (Automatic implantable cardioverter-defibrillator),
B. Beta blocking agents
C. Calcium channel blockers, Coronary revascularization, Cardiac transplant, Cardiomyoplasty, Surgery.
D. Diet, Diuretics, Digitalis, Dobutamine
E. Exercise
Sympathomimetic
· Dopamine, Dobutamine
· Dopamine: Stimulation of peripheral post junctional D1 and pre-junctional D2 receptors.
· Splanchnic (GIT, liver, spleen, and pancreas) and renal vasodilation (increase blood supply).
· Use: Restore renal blood in acute failure.
· Dobutamine: Stimulate β1 adrenoreceptor – Peripheral vasodilatation.
· Use: management of acute failure.
Phosphodiesterase inhibitors
· Amrinone, Milrinone, levosimendan
· Inhibition of type III phosphodiesterase.
· Increase concentration of cAMP leads to activation of protein kinase A.
· Calcium influx through L-type calcium channel.
· Inhibition of calcium sequestration by SR.
Therapeutic uses
· Support I advance cardiac failure (Short term)
· Not for long terms.
Adverse effects
· Cardiac arrhythmia
· Nausea and vomiting
· Thrombocytopenia (low blood platelet count)
· Sudden death
RAS inhibitors
· Drugs of choice in heart failure with diuretics.
· Use: Acute myocardial infraction.
Diuretics
· Reduction of preload and afterload: Reduction of excess plasma volume and edema fluid (Preload), lowered BP (Afterload).
· Reduction facilitation of sympathetic nervous system.
Vasodilators
· Reduce preload and afterload.
· Sodium Nitroprusside, Hydralazine, Ca2+ channel blockers, Prazosin.
β- Blockers
· Blocks the action of Epinephrine and Nor-epinephrine.
· Inhibition of renin release
Aldosterone antagonist
· Prevention of aldosterone effect on kidney and heart.
· Remove edema in heart failure.
· Prolong life in CHF patients.

Hi…!! This is Smrutiranjan Dash, Assistant Professor of Pharmacology from Odisha, India. With a passion for teaching and a dedication to advancing the field of pharmacology, I am committed to sharing knowledge, fostering innovation, and inspiring future healthcare professionals.
About The Author
Hi...!! This is Smrutiranjan Dash, Assistant Professor of Pharmacology from Odisha, India. With a passion for teaching and a dedication to advancing the field of pharmacology, I am committed to sharing knowledge, fostering innovation, and inspiring future healthcare professionals.

It’s a pity you don’t have a donate button! I’d most
certainly donate to this fantastic blog! I suppose for now i’ll settle for book-marking and
adding your RSS feed to my Google account. I look forward to fresh updates and will share this site with my Facebook group.
Talk soon!
http://slkjfdf.net/ – Uaobudohe Osesitaz fed.kqak.alleviatenow.in.bwv.on http://slkjfdf.net/
I’m curious to find out what blog system you have been using?
I’m experiencing some minor security problems with my latest website and I’d like to find something more
safe. Do you have any suggestions?
Asking questions are in fact good thing if you are not understanding anything totally,
however this article provides pleasant understanding even.
Very soon this site will be famous amid all blogging and site-building
visitors, due to it’s good articles
What’s up friends, how is the whole thing,
and what you desire to say regarding this post, in my view its really awesome designed
for me.
My developer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using Movable-type
on numerous websites for about a year and am nervous about switching to
another platform. I have heard very good things about blogengine.net.
Is there a way I can transfer all my wordpress posts into it?
Any help would be really appreciated!
I was wondering if you ever thought of changing
the layout of your website? Its very well written; I
love what youve got to say. But maybe you could a little more in the
way of content so people could connect with it better.
Youve got an awful lot of text for only having 1
or two images. Maybe you could space it out better?
Great post. I was checking continuously this blog and I’m inspired!
Extremely helpful info specially the final section 🙂 I maintain such information much.
I used to be seeking this certain information for a very lengthy time.
Thank you and best of luck.
Hey there are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started and set up my own. Do you
need any html coding knowledge to make your own blog?
Any help would be really appreciated!