Hormone
· Hormone produce intense biological activity that is produced by specific cells in the body and it transported through circulation on its target cells.
Body function | Major regulator hormones |
· Fuel | · Insulin, glucagon, growth hormone |
· Metabolic rate | · Tri-iodothyronine, thyroxine |
· Somatic growth | · Growth hormone, insulin |
· Sex and reproduction | · Gonadotropins, androgens, estrogens, progestin |
· Circulating volume | · Aldosterone, Anti-diuretic hormone |
· Adaptation to stress | · Glucocorticoids, adrenaline |
· Calcium balance | · Parathormone, calcitonin, vitamin D |
· Hormone are secreted by the endocrine or ductless glands; these are:
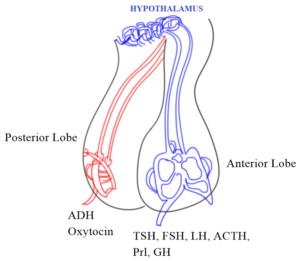
1. Pituitary
a) Anterior lobe:
o Growth hormone (GH), prolactin (Prl), adrenocorticotropic hormone (ACTH, corticotropin), thyroid stimulating hormone (TSH, thyrotropin),
o Gonadotropins: Follicle stimulating hormone (FSH), and luteinizing hormone (LH).
b) Posterior lobe:
o Oxytocin, anti-diuretic hormone (ADH)
1. Thyroid
o Thyroxine (T4), tri-iodothyronine (T3), calcitonin.
2. Parathyroid
o Parathormone (PTH)
3. Adrenals
i. Cortex: Glucocorticoids (hydrocortisone), mineralocorticoids (aldosterone), sex steroids (dehydroepiandrosterone)
ii. Medulla: Adrenalin, Nor-adrenalin
4. Pancreas
o Insulin, glucagon
5. Gonads
o Androgens (testosterone)
o Estrogens (estradiol)
o Progestin (progesterone)
MECHANISM OF HORMONE ACTION
1. At cell membrane receptor | |
Mechanism | Hormones |
a) Alteration of intracellular cAMP → Ca2+ activation (sometime act as third messenger) | Adrenalin, glucagon, TSH, FSH, Vasopressin (V2) |
b) Through IP3/DAG pathway → PKc → Ca2+ | Vasopressin (V1), oxytocin |
c) Direct transmembrane activation of tyrosine protein kinase ↓ Phosphorylation ↓ Regulation of various enzyme | Insulin, GH, prolactin |
2. At cycloplasmic receptors | |
· Penetrating cell membrane, hormone combines with a cytoplasmic receptor ↓ Exposes its DNA binding domain ↓ Migrate to nucleus and binds to specific genes ↓ DNA mediated mRNA synthesis | Steroid hormone: glucocorticoids, mineralocorticoids, androgens, estrogens, progestins, calcitriol |
3. At nuclear receptor | |
· The hormone penetrates the nucleus ↓ Combine with receptor ↓ Alter DNA-RNA mediated protein synthesis | Thyroid hormone: T3, T4 |
PITUITARY
Growth hormone
· It is 191 amino acid single chain peptide, molecular weight 22000
· Increase the size of the body part EXCEPT Brain, Eye (Independent).
· GH acts on the cell surface JAK-STAT protein kinase.
↓ Binding
GH-Receptor (Dimer)
↓
Conformational changes
↓ Activate
JAK-STAT tyrosine protein kinase
↓
Regulate gene expression
· Metabolic action of GH are exerted indirectly through the peptides called somatomedins or Insulin like growth factor (IGF 1-2)
· IGF-Extracellular mediators of GH response
· IGF produced by other target cells promotes lipogenesis and glucose intake by muscle.

Regulation of secretion
· GH secretion increase or decrease by the action of cAMP.
· Somatostatin → inhibit Ca2+channels and open K+ channel.
· Increase plasma free fatty acid → inhibit the secretion of GH
· Dopaminergic agents → increase GH release.
Causes
· Increase GH → Gigantism
· Decrease → Dwarfism
· Hyperlipidemia
Therapeutic uses
· Dwarfism
· Prader-willi syndrome
· Maintain, build and repair of tissues
· Management of AIDs wasting syndrome.
Experimental uses
· Infertility, chronic catabolic state
· Inflammatory bowel disease
· Burn injury
Adverse effects
· Decrease immunogenicity
· Lipodystrophy (Abnormal distribution of fat in the body)
· Glucose intolerance
· Hypothyroidism
· Salt and water retention
· Myalgia (muscle pain)
· Headache
Growth hormone inhibitor
· Somatostatin
· Octreotide
· Lanreotide
· Pegvisomant
PROLACTIN
· It contains 199 amino acid single chain peptide of molecular wt. 23000 (similar to GH).
Physiological function
· It primarily stimulus with the conjunction with estrogen, progesterone and several hormone.
· Prolactin causes development and growth of breast during pregnancy.
· The ductal and acinar cell induce synthesis of milk and lactose.
· Prolactin may affect immune response through action on T-lymphocytes.
· Overproduction of prolactin causes lactational amenorrhea.

Regulation
· Secretion of prolactin is inhibited by dopamine acting at D2 receptors (pituitary lactotrope D2 receptor).
· Dopamine agonist: decrease plasma prolactin level.
· Dopamine antagonist (chlorpromazine, haloperidol, metoclopramide, and reserpine) → causes hyperprolactinemia.
Prolactin inhibitor
1) Bromocriptine
2) Cabergoline
· Decrease prolactin release from pituitary by activating D2 receptor on lactotrope.
· Increase GH release → (Acromegaly)
· CNS → Anti-parkinsonism, behavioral effects (like levodopa)
· Produce nausea and vomiting
· Decrease GIT motility.
Pharmacokinetics
· 1/3 oral dose of the Bromocriptine is absorbed.
· Due to fast pass metabolism bioavailability is lowered.
· Metabolized and excreted in bile.
· Plasma t ½ is 3-6 hours.
Side effects
· In early stage: Nausea, vomiting, constipation, nasal blockade, hypotension.
· Late stage: Behavioral alteration, mental confusion, hallucination, psychosis.
Uses
· Hyperprolactinemia
· Acromegaly
· Parkinsonism
· Diabetic mellitus
· Hepatic comma
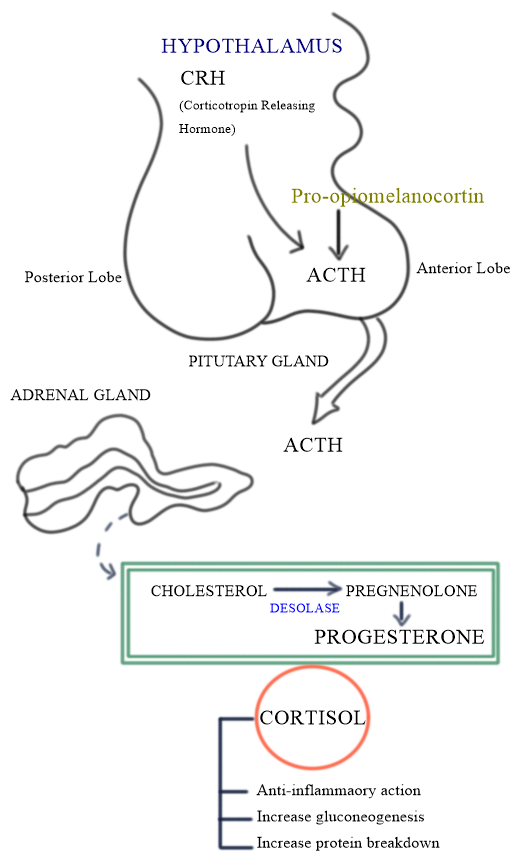
ADRENOCORTICOTROPIC HORMONE (CORTICOTROPIN)
· 39 amino acid single chain peptide, molecular wt. 4500 derived from a large peptide pro-opiomelanocortin (molecular wt. 30000).
Physiological function
· ACTH target adrenal cortex and bind to its specific receptor.
· Activate GPCR and increase cAMP, which turn stimulate adrenocorticoid synthesis pathway – cholesterol → pregnenolone.
· Synthesis and release adrenocorticosteroid and the adrenal androgen.
Therapeutic uses
· Primarily for the diagnosis disorder of pituitary adrenal axis.
· Injected i.v. 25 IU causes increase in plasma cortisol if the adrenal are functional.
· ACTH does not offer because MORE inconvenient, expensive as well as less predictable.
Adverse effects
· Osteoporosis
· Hypertension
· Peripheral edema
· Hypokalemia
· Infection
GONADOTROPINS (GNs)
· Anterior pituitary secrete two GNs
i. FSH (Follicle stimulating hormone)
ii. LH (Luteinizing hormone)
· Both are glycoprotein containing 23-28% sugar and consist of two peptide chains.
· α-Chain: FSH and LH (92 amino acid)
· β-Chain: FSH (111 amino acid), LH (121 amino acid)
FSH
· Female: Includes follicular growth, development of ovum and secretion of estrogens. (FSH receptor is expressed on somniferous sertoli cells).
· Male: Spermatogenesis
LH
· Female: Regulate the length and order of the menstrual cycle.
· Male: Stimulate testosterone secretion.
Role
· Both LH and FSH are GPCR → Activate cAMP production
↓ Stimulates
Gametogenesis
↓ Conversion of
Cholesterol → Pregnenolone

Adverse effects
· Ovarian hyper-stimulation
· Pain in lower abdomen
· Allergies
· Edema
· Headache, mood changes.
Uses
· Amenorrhea and infertility (Non ovulation due to polycystic ovaries).
· Hypogonadism in male
· Cryptorchidism (Testicle fail to descend from the abdomen into the scrotum).
Thyroid and antithyroid drugs
· The thyroid hormone is of two types;
i. Iodine containing amino acids
§ Thyroxine (T4)
§ Triiodothyronine (T3)
ii. Peptides
§ Calcitonin
· The iodine containing amino acids are produced by thyroid follicles and have broad effects on growth, developments and metabolism.
· Calcitonin is produced by interfollicular “C” cells and biologically important in calcium metabolism.
Synthesis and transport of thyroid hormone
1. Iodine uptake
· The iodide is uptake by “Na+ iodide symporter (NIS)” and to concentrate this anion (I2).
· The trapping is stimulated by TSH by inducing and activating NIS.
2. Oxidation and iodination
· Iodide trapping by follicular cells is carried across the apical membrane by the transporter “pendrin” and oxidized by the membrane bound thyroid peroxidase enzyme to linked (I+) ion OR hypoiodus acid (HOI) OR enzyme linked hypoiodate (E-OI) with the help of H2O2.
· These iodines combine with tyrosil residues of thyroglobulin to form;
→ Monoiodotyrosine (MIT) and
→ Diiodotyrosine (DIT)
3. Coupling
· Pairs of iodinated tyrosine residues couple together to form T3 and T4.
· The formation of T4 is much more than T3, but in case of I2 deficiency relatively more MIT is available and more T3 is formed.
· Coupling is an oxidative reaction, hence coupling and oxidation of iodide are stimulated by TSH.
· The same thyroid peroxidase is catalyzed the reaction of coupling.
4. Storage and release
· Thyroglobulin containing iodinated tyrosil and thyronil residue is transported to the interior of the follicles and remains stored as thyroid colloid.
· The coupling residue is taken back into the cells by endocytosis and broken down by lysosomal proteases to form T4 and T3.
· The T4 and T3 is then secreted into the circulation.
· Both colloid uptake and proteolysis are stimulated by TSH.
5. Peripheral conversion of T4 to T3
· Peripheral tissues like liver and kidney convert T4 to T3.
· The target tissues take up T3 from circulation and T4 is taken up by brain and pituitary and converts T4 to T3 with in their own cells.
· The same amount of T3 and reverse T3 (rT3) are produced in the periphery.
· The conversion of T4 to T3 is carried out by the enzyme iodothyronine deiodinase which exists in 3 forms; that is D1, D2, and D3.
→ D1: generates both T3 and rT3 (Propylthiouracil block D1 form)
→ D2: generates T3 (Amiodarone)
→ D3: generates rT3 (Amiodarone)
→ Conversion of T4 to T3 (Propranolol high dose)

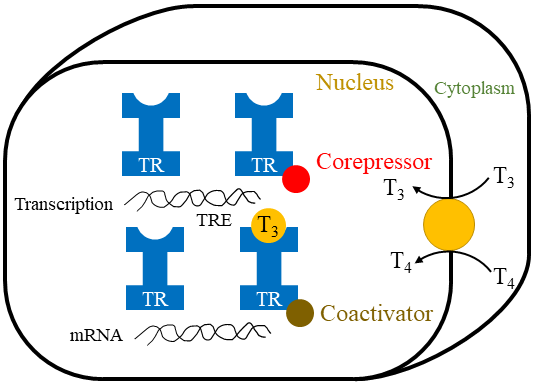
MECHANISM OF ACTION
· Both T3 and T4 penetrate cells by active transport and combining with a nuclear thyroid hormone receptor (TR) → (Steroid and Retinoid).
· Steroid receptor: the TR residues in the nucleus even in the unliganded inactive state.
· It bound to thyroid hormone response element (TRE) along with corepressors.
· When T3 binds to the ligand-binding domain of TR, it heterodimerizes with retinoid X receptor (RXR), undergoes conformational changes induces gene transcription and production of protein synthesis.
PHARMACOKINETICS
· Nearly 75% oral bioavailability.
· Severe hypothyroidism may reduce oral absorption.
· Administration in empty stomach.
· Sucralfate, Iron, Calcium and Proton Pump Inhibitor inhibit L. thyroxine absorption.
· Rifampin, Phenytoin, and Carbamazepine (CYP3A4 inducer) accelerate metabolism of T4.
USES
1. Cretinism
· Severe physical and mental retardation.
· Treatment thyroxine (8-12 microgram/kg) as early possible.
2. Myxedema
· Low HR
· Weight gain
· Weakness
· Goiter
3. Myxedema coma
· Loss of brain function
4. Nontoxic goiter
· Nodular enlargement of the thyroid gland.
5. Thyroid nodule
· Solid or fluid filled lumps.
· Most thyroid nodules are not serious and don’t cause symptoms.
6. Papillary carcinoma of thyroid.
· A cancer of the thyroid.
7. Empirical uses
· Also, T4 has been used in
→ Refractory anemias
→ Mental depression
→ Menstrual disorder
→ Chronic / non-healing ulcer
→ Obstinate constipation

Hi…!! This is Smrutiranjan Dash, Assistant Professor of Pharmacology from Odisha, India. With a passion for teaching and a dedication to advancing the field of pharmacology, I am committed to sharing knowledge, fostering innovation, and inspiring future healthcare professionals.
About The Author
Hi...!! This is Smrutiranjan Dash, Assistant Professor of Pharmacology from Odisha, India. With a passion for teaching and a dedication to advancing the field of pharmacology, I am committed to sharing knowledge, fostering innovation, and inspiring future healthcare professionals.

Im very pleased to find this site. I need to to thank you for ones time for this particularly fantastic read!! I definitely really liked every part of it and I have you bookmarked to see new information on your site.
I need to to thank you for this good read!! I certainly enjoyed every bit of it. I have you saved as a favorite to look at new things you postÖ
I congratulate, a brilliant idea