ROUTES OF DRUG ADMINISTRATION
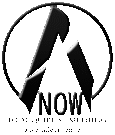
Routes of drug administration are defined as the various pathways or methods through which pharmaceutical agents are introduced into the body to elicit either localized or systemic therapeutic effects.
1. By Extent of Action
A. Systemic Routes
Reach the bloodstream and act throughout the body.
1. Enteral routes
· Oral
· Sublingual
· Rectal
2. Parenteral routes
· Injections
· Intravenous
· Intramuscular
· Subcutaneous
· Intra-arterial
· Intra-articular
· Intrathecal
· Intradermal
· Inhalational
· Transdermal
B. Local Routes
Produce an effect mainly at the site of application.
· Skin topical
· Intranasal
· Ocular (eye) drops
· Mucosal
· Throat
· Vagina
· Mouth
· Ear
· Inhalational
· Transdermal
FACTOR GOVERNING THE CHOICE OF ROUTE
1. Drug properties
- Physical form: Whether the drug is a solid, liquid, or gas determines if it can be given orally, inhaled, or injected.
- Solubility and stability: Drugs that are poorly water-soluble or unstable in gastric acid may need parenteral, sublingual, or transdermal routes.
- pH and irritancy: Highly irritant or very acidic/alkaline drugs may damage skin or mucosa and therefore must be given by a route that minimizes local injury (e.g., deep I.M. instead of S.C.).
2. Site and type of action
- Local action: When effect is required at a specific site (eye, skin, throat), local routes such as topical, ocular, or inhalational are preferred to limit systemic exposure.
- Systemic or generalized action: For actions needed throughout the body (antibiotics, antihypertensives), systemic routes (oral, I.V., etc.) are chosen, especially when the target site is not directly approachable.
3. Absorption characteristics
- Rate of absorption: Routes like intravenous give an immediate effect, while oral or transdermal routes produce slower, more sustained absorption.
- Extent of absorption: Some routes have variable or incomplete absorption (e.g., rectal, oral in the presence of food), which influences dose and reliability of effect.
4. Effect of GIT and first‑pass metabolism
- Digestive juices and enzymes: Acid, enzymes, and bile may degrade sensitive drugs (e.g., some peptides), making oral administration unsuitable.
- First‑pass hepatic metabolism: Drugs extensively metabolized in the liver after oral absorption may show low bioavailability, so alternative routes such as sublingual, transdermal, or parenteral are chosen.
5. Required speed of response
- Emergencies: Conditions like anaphylaxis, cardiac arrest, or acute asthma require a very rapid onset; intravenous or inhalational routes are preferred.
- Routine or chronic therapy: For long-term management (e.g., hypertension, diabetes), convenient routes such as oral or transdermal are favored even if onset is slower.
6. Accuracy and control of dosage
- High precision needed: Intravenous infusion allows very accurate control of dose and blood levels, important for drugs with a narrow therapeutic index.
- Less critical dosing: When small fluctuations are acceptable, oral or other convenient routes are used, even if absorption varies somewhat.
7. Patient’s condition and cooperation
- Consciousness and swallowing ability: Unconscious, vomiting, or uncooperative patients cannot take oral drugs, so parenteral, rectal, or transdermal routes are preferred.
- Age and special populations: Paediatrics, geriatrics, or patients with severe pain or phobia of injections may need modified routes (e.g., oral liquids, suppositories, patches) to improve comfort and adherence.
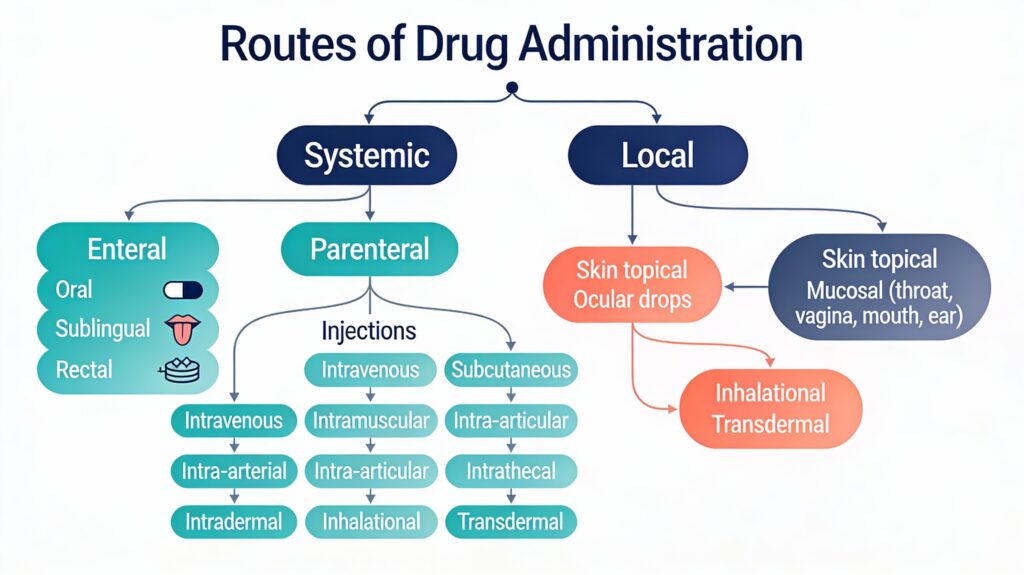
ORAL ROUTE
- Oral route means the drug is taken by mouth and swallowed, so it passes through the gastrointestinal (GI) tract before absorption.
- It is the most commonly used route in clinical practice because it suits long‑term therapy and outpatient use.
Key advantages
- Safe: Generally, the safest route because drug entry is slower and, if needed, the drug can sometimes be removed (induced vomiting, gastric lavage, activated charcoal).
- Convenient: Patients can self-administer tablets, capsules, or liquids at home without medical help, so treatment becomes pain-free, non-invasive, and easy to continue for chronic diseases.
- Economical: Oral formulations are cheaper to manufacture and administer than most injectable preparations, reducing overall treatment cost.
- Good absorption: The drug can be absorbed at multiple sites (stomach, small and large intestine), giving a large effective surface area and usually satisfactory bioavailability for many drugs.
- No sterilization required: Unlike injections, oral solid and liquid preparations do not need to be sterile, which simplifies production and storage and lowers cost.
Key Disadvantages
- Slow absorption and onset: Drug must disintegrate, dissolve, and pass through the GI tract, leading to 30 minutes to 2-hour delay—unsuitable for emergencies like cardiac arrest or severe pain.
- Nausea/vomiting and unpalatable drugs: Patients with nausea, vomiting, or motion sickness cannot retain tablets; bitter or large tablets reduce compliance.
- Unconscious or uncooperative patients: Comatose, post-operative, or paediatric patients unable to swallow safely require alternative routes like IV or rectal.
- Destruction by GI secretions: Acid-labile drugs (e.g., penicillin G, insulin) or enzyme-sensitive peptides are degraded in stomach acid or intestinal enzymes before absorption.
- Inefficient or variable absorption: Some drugs have poor bioavailability (e.g., due to pH changes, food effects, or disease states like diarrhea), requiring higher doses.
- First-pass metabolism: Orally absorbed drugs pass through the liver via the portal vein, undergoing extensive metabolism (e.g., propranolol, morphine), reducing systemic availability.
- Food-drug and drug-drug interactions: Food delays gastric emptying and absorption; drugs like tetracycline bind to dairy calcium, while antacids alter pH and reduce efficacy of others.
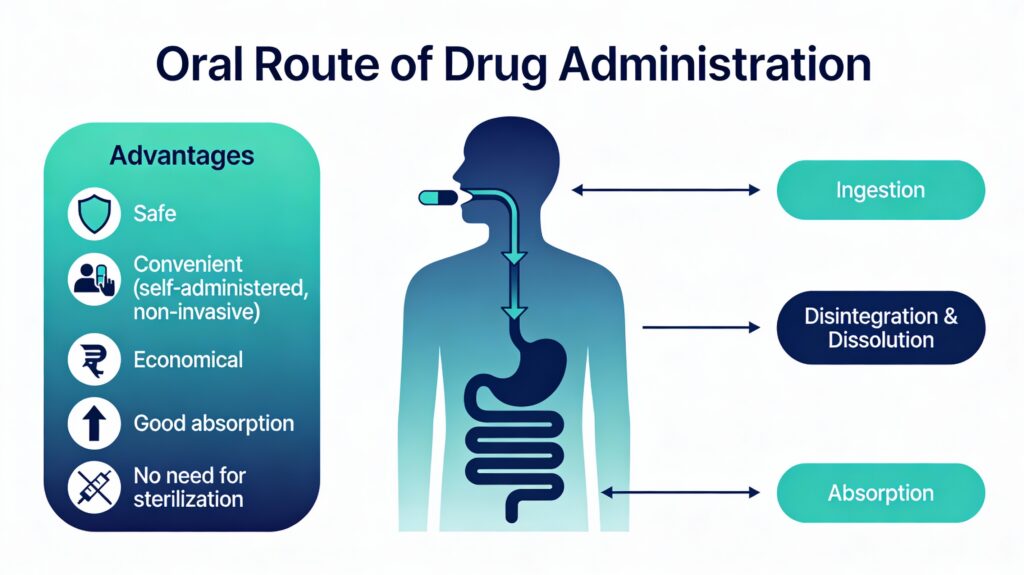
SUBLINGUAL OR BUCCAL ROUTE
A tablet, pellet, or spray containing the drug is placed under the tongue (sublingual) or against the buccal mucosa (buccal) and held until dissolved. Examples include glyceryl trinitrate (GTN) for angina, buprenorphine for pain, and desmopressin or oxytocin sprays.
Advantages
- Quick absorption: Highly vascular oral mucosa allows fast entry into systemic circulation (onset in 1-5 minutes), ideal for acute conditions like angina attacks.
- Quick termination: The effect can be stopped by swallowing or spitting out the tablet if an overdose occurs.
- First-pass avoided: Drugs bypass the liver initially via absorption into the jugular vein, achieving higher bioavailability for drugs like GTN that undergo extensive hepatic metabolism.
- Self-administered: Easy for patients to use at home without needles or supervision.
Disadvantages
- Unpalatable and bitter drugs: Many drugs (e.g., nitroglycerin) have an unpleasant taste, limiting patient acceptance.
- Irritation of oral mucosa: Prolonged contact can cause local soreness or ulceration with repeated use.
- Large quantities not possible: Limited surface area restricts dose size; only small amounts (a few mg) can be absorbed effectively.
- Few drugs are suitable: Only lipid-soluble, non-irritant drugs with low molecular weight work well; most drugs are formulated for oral or other routes.
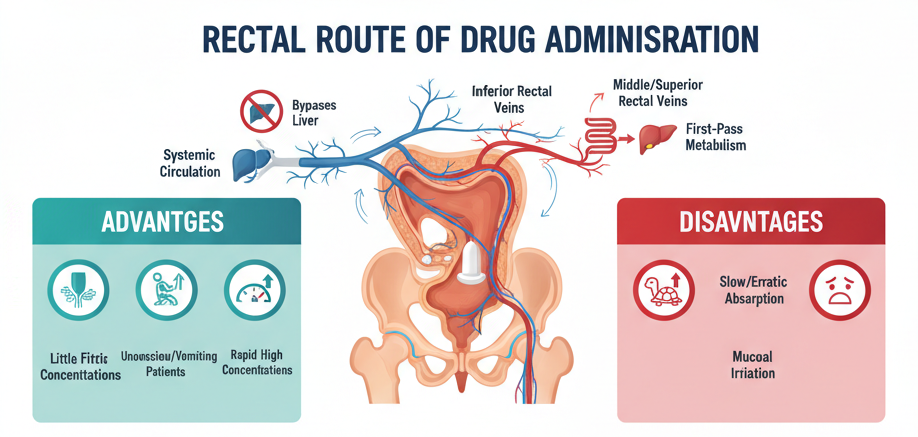
RECTAL ROUTE
Suppositories melt at body temperature or disperse in rectal fluid, releasing the drug for local or systemic absorption. Examples include diazepam (seizures), indomethacin (pain), paraldehyde (convulsions), and ergotamine (migraine).
Advantages
- Little or no first-pass effect: Lower rectal veins drain directly into systemic circulation (inferior vena cava), bypassing liver metabolism, unlike the oral route.
- Useful in haemorrhoidal vein cases: Effective for patients with liver disease where hepatic metabolism is impaired.
- High concentrations rapidly achieved: Absorption can be faster than oral for some drugs, suitable for unconscious or vomiting patients (e.g., paediatric seizures).
Disadvantages
Aspect | Description |
Absorption | Often slow and erratic; incomplete or variable bioavailability |
Patient Factors | Inconvenient, embarrassing; requires patient positioning and retention |
Local Effects | Irritation, inflammation, or proctitis of the rectal mucosa is possible |
Formulation Limits | Suppositories may expel before full absorption; limited drug compatibility |
· The rectal route suits emergencies when oral/IV is unavailable, but is less common due to compliance issues.
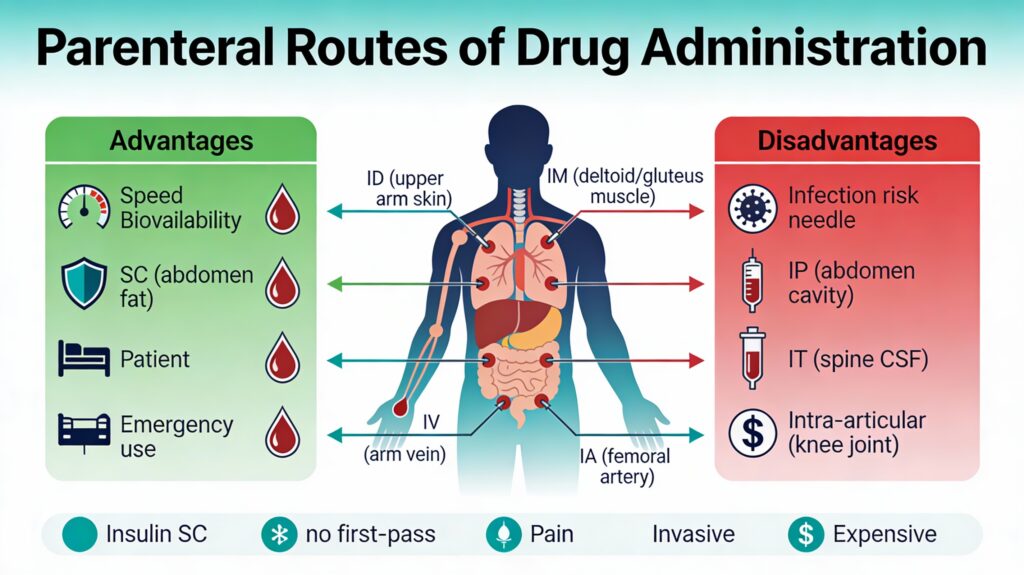
PARENTERAL ROUTE
Parenteral administration bypasses intestinal mucosa barriers, first-pass metabolism, and gastrointestinal degradation, making it ideal for emergencies, unconscious patients, or unstable drugs that are not orally stable. Requires sterile technique to prevent infections.
Types of Parenteral Routes
|
Route (Abbreviation) |
Site of Administration |
Onset & Use Cases |
|
Intradermal (ID) |
Into the skin (dermis layer) |
Slow; allergy tests, vaccines (e.g., TB test) |
|
Subcutaneous (SC) |
Into the subcutaneous fat |
Moderate; insulin, heparin (e.g., diabetes management) |
|
Intramuscular (IM) |
Into skeletal muscle |
Fast; vaccines, antibiotics (e.g., tetanus toxoid) |
|
Intravenous (IV) |
Into veins |
Immediate; emergencies, infusions (e.g., fluids, chemotherapy) |
|
Intra-arterial (IA) |
Into arteries |
Very rapid/local; angiography, cancer therapy |
|
Intrathecal (IT) |
Into the spinal canal (CSF) |
Rapid CNS; spinal anesthesia, chemotherapy |
|
Intraperitoneal (IP) |
Into the peritoneal cavity |
Moderate; chemotherapy, dialysis |
|
Intra-articular (IA) |
Into the synovial joint fluid |
Local: arthritis steroids |
Advantages
- Rapid and complete bioavailability: Immediate onset (especially IV), 100% absorption without GI barriers or first-pass metabolism.
- Suitable for emergencies/unconscious patients: Ideal when oral intake is impossible (e.g., nausea, coma) or precise dosing is needed (e.g., insulin SC).
- Versatile for drug types: Handles irritant, unstable, or large-volume drugs unsuitable for oral administration.
Disadvantages
|
Aspect |
Key Issues |
|
Safety Risks |
Invasive; infection, pain, tissue damage, nerve injury possible |
|
Technical Needs |
Requires skilled administration, sterility; irreversible once given |
|
Cost & Comfort |
Expensive formulations; higher patient discomfort vs. oral routes |
INTRAVENOUS ROUTE
The intravenous (IV) route delivers drugs directly into veins for immediate systemic circulation, bypassing first-pass metabolism and GI absorption barriers.
Advantages
- 100% bioavailability: Complete and instantaneous drug delivery without losses from absorption or hepatic metabolism.
- Precise control: Allows titration of dose levels, rapid adjustment for therapeutic response, and administration of large volumes.
- Pain-free and versatile: Suitable for emergencies, unconscious patients, or drugs unsuitable for other routes; avoids the first-pass effect.
Disadvantages
- Too rapid delivery risks: High concentrations can cause sudden toxicity, anaphylaxis, or cardiac arrhythmias.
- No recall possible: Unlike oral drugs, IV effects cannot be reversed by emesis or charcoal if overdosed.
- Local/systemic complications: Thrombophlebitis, vein necrosis, hemolysis, embolism; requires sterile technique to prevent infections.
INTRAMUSCULAR ROUTE
The intramuscular (IM) route injects drugs into large skeletal muscles like the deltoid, triceps, gluteus maximus, or rectus femoris for reliable absorption into systemic circulation.
Advantages
- Reasonably uniform rapid onset: Absorption faster than subcutaneous (15-30 min onset), suitable for moderately urgent needs like antibiotics or vaccines.
- Mild irritants tolerated: Larger blood supply handles irritating drugs better than SC sites.
- First-pass avoided; gastric factors bypassed: No GI degradation or hepatic first-pass; unaffected by food or nausea.
Disadvantages
Issue | Description |
Volume limitation | Only up to 10 mL (2-5 mL preferred); larger risks of tissue damage |
Local complications | Pain, abscess, sterile abscess at the injection site |
Systemic risks | Nerve damage (sciatic in the gluteal), hematoma in anticoagulated patients |
Subcutaneous (SC) route injects drugs into the fatty layer beneath the skin, providing slower absorption than IM due to less vascular supply; suitable for irritant drugs in small volumes.
Key Features
- Volume limitation: Only small volumes (up to 1-2 mL) can be injected to avoid discomfort or tissue distortion.
- Depot preparations: Sustained-release forms like dermojet, pellets, silastic implants, or biodegradable implants for long-term therapy (e.g., insulin, hormones).
- Related routes:
- Intradermal (ID): Into skin, raising a bleb for tests (BCG vaccine, sensitivity tests).
- Intrathecal/Intraventricular: Into the subarachnoid space/CSF for CNS infections (e.g., amphotericin B for cryptococcal meningitis).
Advantages and Disadvantages
Advantages | Disadvantages |
Slow, sustained absorption is ideal for chronic therapy | Slower onset than IM/IV; unsuitable for emergencies |
Self-administerable (e.g., insulin pens) | Limited volume; irritants cause pain/abscess |
Bypasses GI/first-pass; good for peptides | Variable absorption if circulation is poor (e.g., shock) |
TRANSDERMAL ROUTE
The transdermal route achieves systemic effects by applying drugs to intact skin, typically via medicated adhesive patches that allow slow diffusion through skin layers into circulation.
Key Features
- Drug characteristics: Requires lipophilic drugs with suitable physical properties for skin permeation; applied to sites like the upper arm or chest.
- Examples: Nicotine patches (smoking cessation), nitroglycerin (angina), scopolamine (motion sickness).
- Absorption enhancement: Oily cleansing preparations increase permeation; first-pass metabolism is avoided.
Advantages and Disadvantages
Advantages | Disadvantages |
Slow, prolonged action (24-72 hrs) for sustained delivery | Only lipophilic, low MW drugs are suitable; poor for hydrophilic drugs |
First-pass bypassed; steady blood levels without peaks/troughs | Skin irritation and allergy at the application site are common |
Self-administered, convenient for chronic therapy | Slow onset (hours); unsuitable for acute/emergency use |
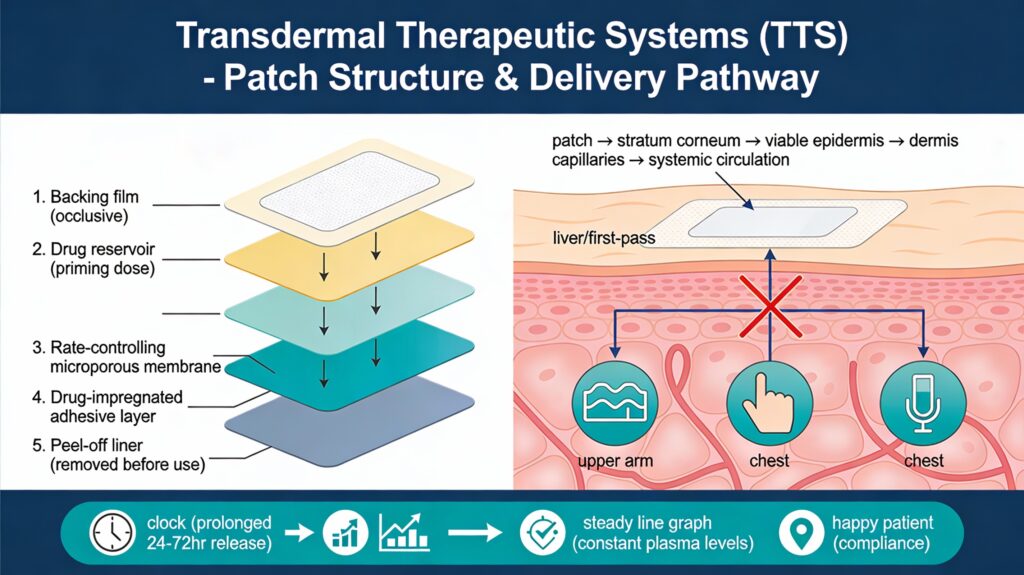
TRANSDERMAL THERAPEUTIC SYSTEMS
Transdermal therapeutic systems (TTS) are multilayered adhesive patches applied to skin (e.g., upper arm, chest, mastoid region) for controlled, sustained systemic drug release through intact skin.
Patch Structure
- Backing film: Occlusive drug-impermeable layer protects contents.
- Drug reservoir: Contains priming dose in solution or matrix.
- Rate-controlling microporous membrane: Regulates diffusion.
- Adhesive layer: Impregnated with drug; secures patch to skin (peel-off film removed just before application).
Advantages
- Steady plasma concentrations: Avoids fluctuations of oral dosing; first-pass bypassed for better bioavailability.
- Improved compliance: Convenient, once-daily/weekly application enhances patient adherence for chronic therapy (e.g., nicotine, nitroglycerin).

With a foundation in pharmacology, I am engaged in both teaching and research. My work has been published in reputed national and international journals, and I actively participate in scientific conferences to share findings and stay connected with emerging advancements. Thank you for visiting. Your interest is truly appreciated.